MAP TITLE: Tackling obesity in the UK(Node #340964)With concern growing that the Foresight analysis—that 50% of the UK population could be obese by 2050, at an annual cost to the nation of around £50 billion per year [2]—substantially underestimates the scale of the unfolding obesity crisis, the College of Contemporary Health is working with the wider policy community to develop a whole systems map of the obesity crisis and the potential responses.
Short Link: debategraph.org/obesity Register/log-in
Outline view ›› Document view ›› Radial view ›› Add a Comment or Link ››
In introducing their excellent recent analysis [7] of the obesity challenge in the UK and beyond, the McKinsey Global Insight authors noted:
...our analysis is by no means complete. Rather, we see our work on a potential program to address obesity as the equivalent of the maps used by 16th-century navigators. Some islands were missing and some continents misshapen in these maps, but they were still helpful to the sailors of that era. We are sure that we have missed some interventions and over- or underestimated the impact of others. But we hope that our work will be a useful guide and a starting point for efforts in the years to come, as we and others develop this analysis and gradually compile a more comprehensive evidence base on this topic.
Similarly, the authors of the 2007 Foresight Report [2] engaged in extensive systems mapping work to develop a qualitative, causal loop model to:
- help us understand the complex systemic structure of obesity
- contribute to developing a tool that helps policy makers respond to obesity in the generation, definition and testing of possible policy options.
The obesity mapping project initiated here by The College of Contemporary Health [8] is grounded the same spirit and intent. It aims to create a comprehensive and coherent visual representation of the obesity governance space – including the causes, impacts, policy actors, proposed interventions, evidence, guidance, and barriers to change – that can help each stakeholder explore and understand the space as a systemic whole; that can be collaboratively and iteratively edited, refined, and evaluated by the policy community; and that provides a dynamic, open substrate for dialogue, learning and action across the policy community.

Obesity Mapping Project initiated by The College of Contemporary Health
Causes of obesity(Node #348780)Understanding the causes of obesity is critical to the success of prevention and treatment strategies. However, while (simply put) obesity occurs when energy intake from food and drink consumption is greater than energy expenditure through the body’s metabolism and physical activity over a prolonged period (resulting in the accumulation of excess body fat), in reality many complex behavioural and societal factors contribute systemically to the current crisis and no single influence dominates.

View full size >>
The Foresight report [2] refers to a “complex web of societal and biological factors that have, in recent decades, exposed our inherent human vulnerability to weight gain”, and presents an obesity system map (above) with energy balance at its centre and over 100 variables directly or indirectly influencing this energy balance; grouped in 7 cross-cutting themes (below):
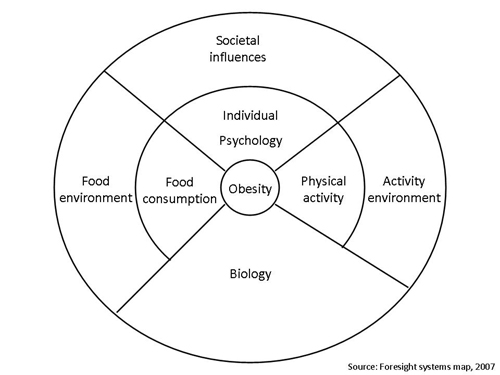
- Biology: an individual's starting point - the influence of genetics and ill health;
- Activity environment: the influence of the environment on an individual’s activity behaviour, for example a decision to cycle to work may be influenced by road safety, air pollution or provision of a cycle shelter and showers;
- Physical Activity: the type, frequency and intensity of activities an individual carries out, such as cycling vigorously to work every day;
- Societal influences: the impact of society, for example the influence of the media, education, peer pressure or culture;
- Individual psychology: for example a person’s individual psychological drive for particular foods and consumption patterns, or physical activity patterns or preferences;
- Food environment: the influence of the food environment on an individual’s food choices, for example a decision to eat more fruit and vegetables may be influenced by the availability and quality of fruit and vegetables near home; and,
- Food consumption: the quality, quantity (portion sizes) and frequency (snacking patterns) of an individual’s diet.
The Government supports the Foresight view that while achieving and maintaining calorie balance is a consequence of individual decisions about diet and activity, our environment (and particularly the availability of calorie-rich food) now makes it much harder for individuals to maintain healthy lifestyles – and that it is for Government, local government and key partners to act to change the environment to support individuals in changing their behaviour.
Obesity takes time to develop and excess weight takes time to be lost. The risks of becoming obese may also start at an early stage. Growth patterns in the first few weeks and months of life affect the risk of later obesity and chronic disease. There is therefore a life-course component.
Tim Lang and Geof Rayner view the current obesity problem in the UK as the result of ‘societal, technical and ideological change' in the last half-century since the end of World War II and, while acknowledging that the present situation is partially a result of a culture in which highly calorific food is available at pocket money prices and technological advances that have made us a more sedentary nation, note also that:
‘the culture of clever and constant advertising flattering choice; the shift from meal-time eating to permanent grazing; the replacement of water by sugary soft drinks; [and] the rising influence of large commercial concerns framing what is available and what sells’ has powerfully contributed to the growing obesity problem.
Genetic susceptibility to an obesogenic environment(Node #373987)Roughly 70 percent of obesity risk is genetically inherited; however, this genetic inheritance is best understood as a susceptibility to a fattening environment––i.e. in a healthy environment, genes alone do not usually cause obesity: in an unhealthy environment, genetically susceptible people become obese, while others remain lean because they are not genetically susceptible. [1]
- The physical and psychological drivers inherent in human biology mean that the vast majority of people are predisposed to gaining weight. We evolved in a world of relative food scarcity and hard physical work rather than the modern world, where energy-dense food is abundant and labour-saving technologies and sedentary life patterns abound. [5]
- The predisposition (by phenotype) to lay down fat is an evolutionary genetic legacy; with the GAD2 gene (on chromosome 10, human genome) appearing to interact with, and speed up, brain neurotransmitters, which in turn activate part of the hypothalamus, stimulating people to eat more. [6]
- However, moving from a genetic predisposition to obesity itself generally requires some change in diet, lifestyle, or other environmental factors. [7]
Industrial way of life is obesogenic(Node #352390)Rapid societal changes—for example, in food production, motorised transport and work/home lifestyle patterns—have placed human physiology (which has evolved to cope with an under-supply of food and high energy expenditure) under new stresses, and revealed an underlying genetic tendency to accumulate and conserve energy (i.e. gain weight) in a high proportion of the population. In this sense, obesity can be construed as a normal physiological response to an abnormal environment.
"The unhealthiest foods have also become, systematically, the: tastiest, cheapest, largest portion-ed, most accessible, most available, most marketed, and most fun foods." [6]
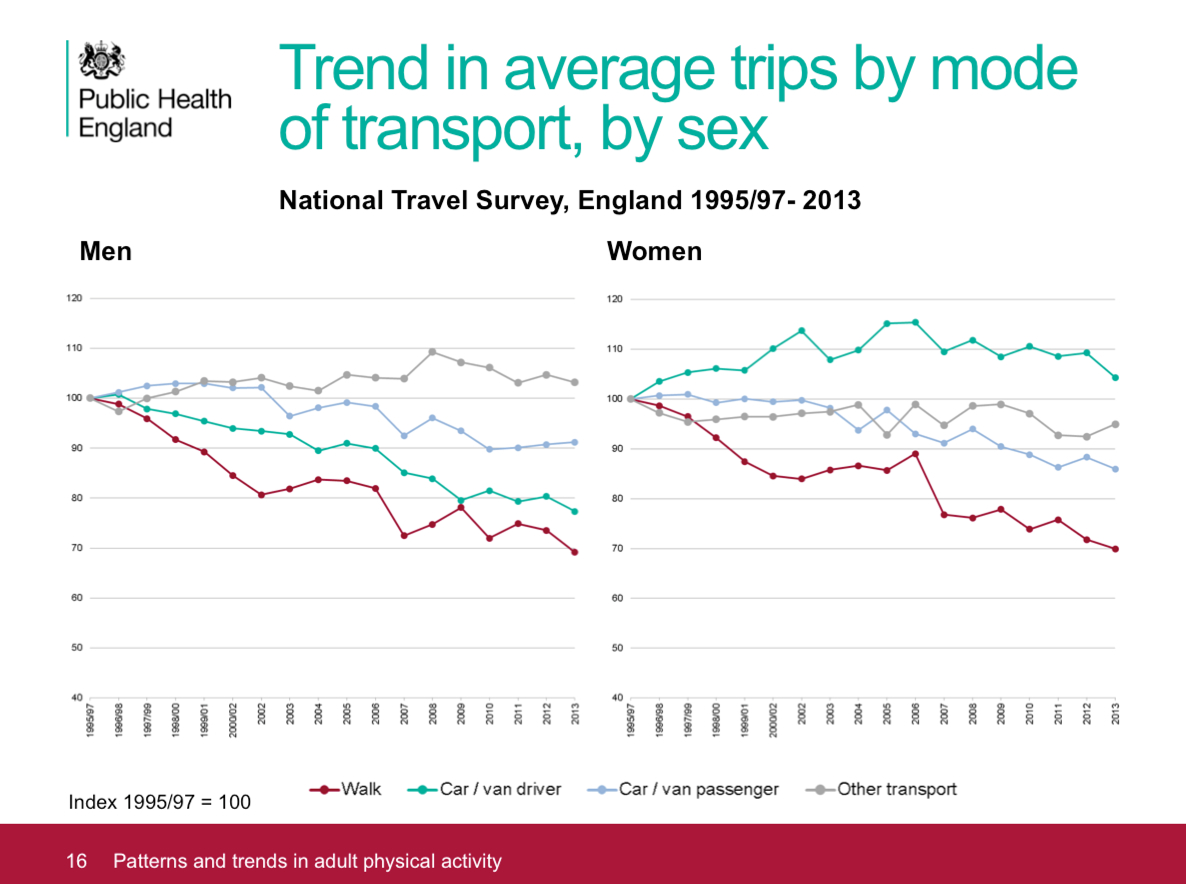
Changing patterns of physical activity(Node #371611)Technological development and urbanisation bring significant shifts in the patterns of daily activity that can reduce the amount of energy people expend in their normal daily routines.
Slides: PHE Adult physical activity slide set – July 2015 [5]Snowdon [6] notes:
If one looks at day-to-day exercise and occupational physical activity, it becomes clear that lifestyles have become more sedentary. The transition from manual labour to office work saw jobs in agriculture decline from eleven to two per cent of employment in the twentieth century while manufacturing jobs declined from 28 to 14 per cent of employment (Lindsay, 2003) [4]. Britons are walking less (from 255 miles per year in 1976 to 179 miles in 2010) and cycling less (from 51 miles per year in 1976 to 42 miles in 2010).
Only 18 per cent of adults report doing any moderate or vigorous physical activity at work while 63 per cent never climb stairs at work and 40 per cent spend no time walking at work (British Heart Foundation, 2012b: 58-59) [3]. Outside of work, 63 per cent report spending less than ten minutes a day walking and 53 per cent do no sports or exercise whatsoever (ibid.: 52-4). Add to this the ubiquity of labour-saving devices and it is clear that Britons today have less need, and fewer opportunities, for physical activity both in the workplace and at home."
Increasingly sedentary lifestyles(Node #348699)Sedentary behaviour is not simply a lack of physical activity but is a cluster of individual behaviours in which sitting or lying is the dominant mode of posture and energy expenditure is very low. Research suggests that sedentary behaviour is associated with poor health in all ages independent of the level of overall physical activity. Spending large amounts of time being sedentary may increase the risk of some adverse health outcomes, even among people who are active at the recommended levels.
The Sedentary Behaviour and Obesity Expert Working Group [2] noted:
- Researchers have increasingly shown an interest in very low levels of movement and sitting, i.e., sedentary behaviour. While the obvious examples of such behaviours are TV viewing and playing computer games, there are many daily sitting behaviours, including car travel, socialising, reading, and listening to music, as well as long periods spent sitting at school or work. It is all of these sedentary behaviours that are of interest to health researchers and policy makers.
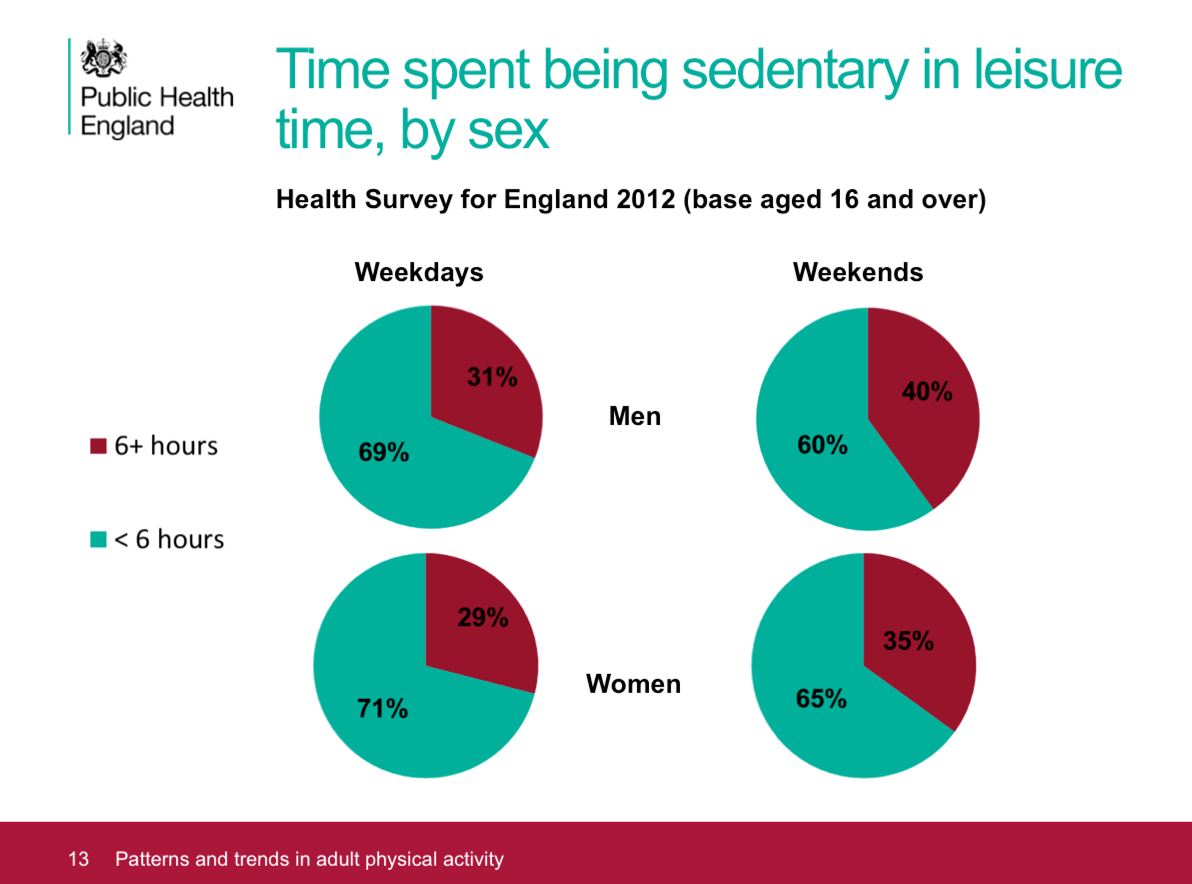
- However, the rise in the interest in sedentary behaviours is closely associated with the rapid increase in the availability and attractiveness of a wide range of screen-based behaviours, including school/work use of computers, leisure time computer use (games, online shopping, internet surfing etc), and TV viewing. While some of these behaviours will have replaced other sedentary pastimes (e.g., radio, reading) over the years, there is widespread belief that the ubiquitous nature of screens is a threat to health from the point of view of very low energy expenditure and hence a risk to the development of overweight and obesity.
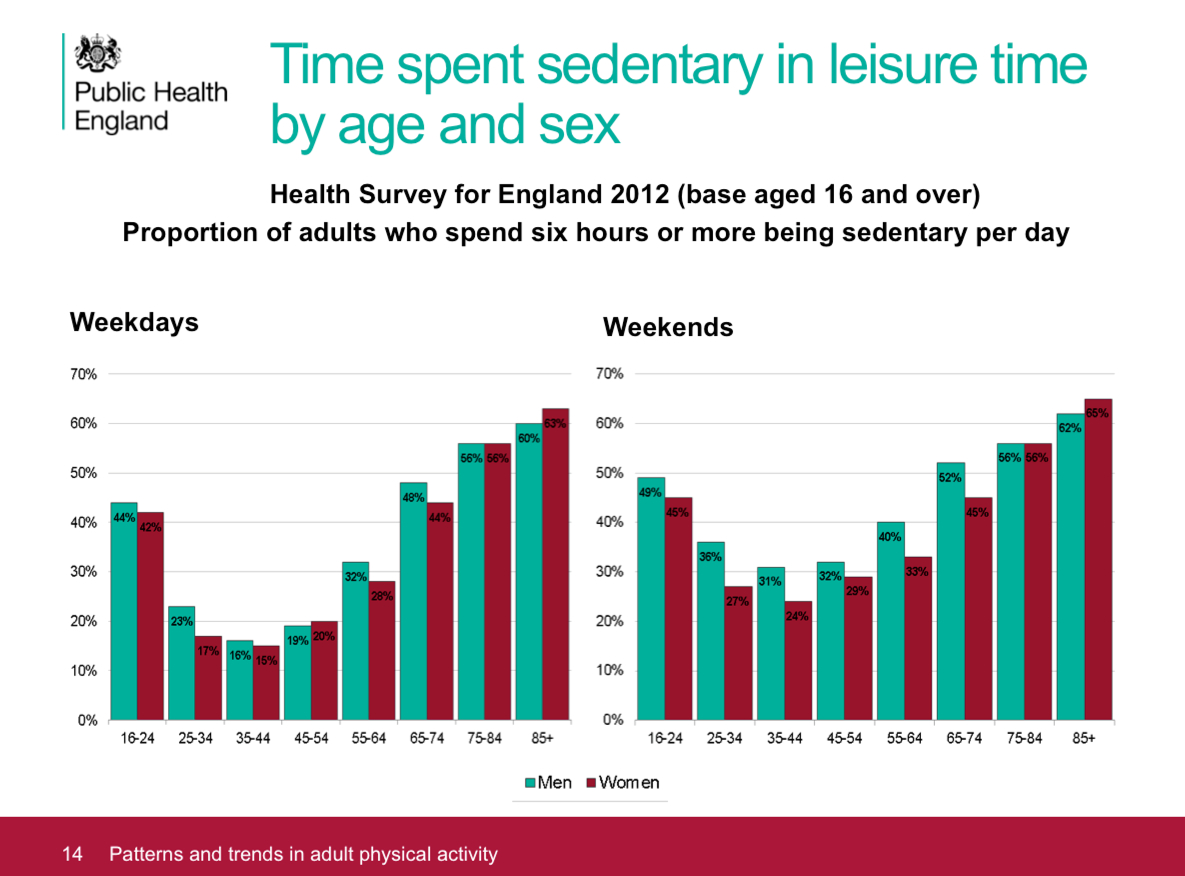
Slides: PHE Adult physical activity slide set – July 2015 [5] TV viewing and obesity(Node #352523)
There’s strong evidence that the more television adults and children watch, the more likely they are to gain weight or become overweight or obese.
Previous physical activities replaced by industrially generated energy(Node #352387)Industrial development allows many different aspects of life that previously involved daily physical activity to be accomplished through industrially generated energy instead; for example, the substitution of motorised transport for walking and cycling, a shift from manual and agricultural work towards office work, and a multitude of labour saving devices at work and in the home.
Slides: PHE Adult physical activity slide set – July 2015 [5] Industrial development changes what and how people eat(Node #352391)
Economic and industrial development has tended to be accompanied by a historic shift in patterns of food consumption from diets high in cereal and fibre to diets high in sugars, fat, animal-source food and highly-processed foods – creating a socio-cultural environment in which obesity is more likely to emerge in the population.
Chronic stress(Node #371614)
The chronically stressful patterns and challenges of modern industrial life trigger bio-physical changes in the hypothalamic–pituitary–adrenal system, which, in combination with more energy being consumed than expended, appear to be a contributor to the increased risk for obesity, especially upper body obesity, and other metabolic diseases.
Reduced sleep(Node #371707)Emerging evidence suggests that people who get insufficient sleep have a higher risk of weight gain and obesity than people who get seven to eight hours of sleep a night.
Reduced sleep may decrease energy expenditure(Node #371711)
Tiredness from reduced sleep may curb physical activity during the day(Node #371713)
People who have insufficient sleep are more tired during the day, and as a result may curb their physical activity.
Reduced sleep may increase energy intake(Node #371710)
Reduced sleep gives people more waking time to eat(Node #371712)
Fewer hours of sleep increases the waking time in which people have to eat.
Reduced sleep may increase hunger(Node #371709)
Sleep deprivation may alter the hormones that control hunger (increasing the appetite-stimulating hormone ghrelin and lowering the levels of the satiety-inducing hormone leptin).
Obesogenicity(Node #373989)
The obesogenicity of an environment is the sum of influences that the surroundings, opportunities, or conditions of life have on promoting obesity in individuals or populations’. [1], [2].
Many individuals are consuming more energy than they are expending(Node #352400)
Public Health England estimates that the average man in England is consuming around 300 calories a day more than they would need were they a healthy body weight.
Not building exercise into daily life (Node #352521)A primary cause of the rise in obesity in the UK in recent decades has been a decline in energy expended rather than rise in energy intake; with the changing pattern towards more sedentary lifestyles appearing to be a key factor in this.
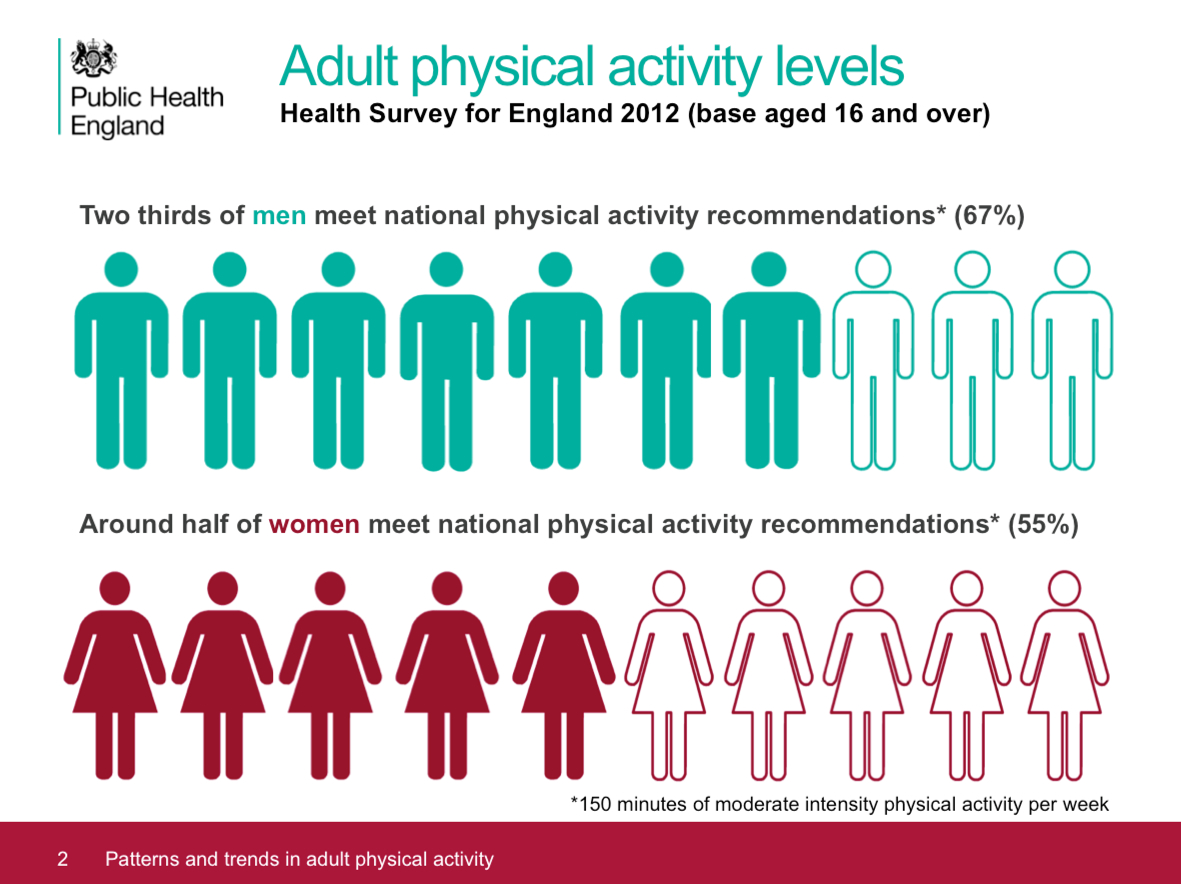
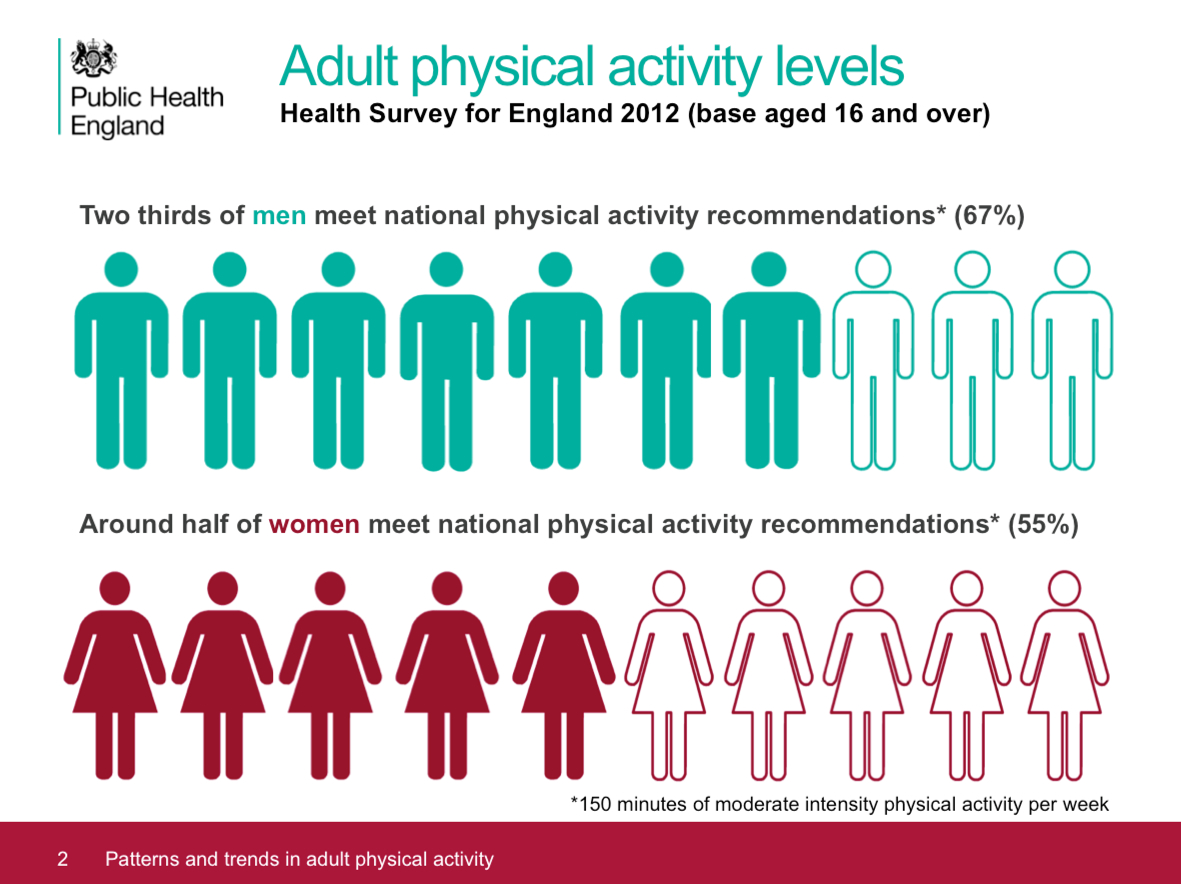
Slide: PHE Adult physical activity slide set – July 2015 [6]Around one in two women and a third of men in England are damaging their health through a lack of physical activity. [8]
- over one in four women and one in five men do less than 30 minutes of physical activity a week, so are classified as ‘inactive’. [2]
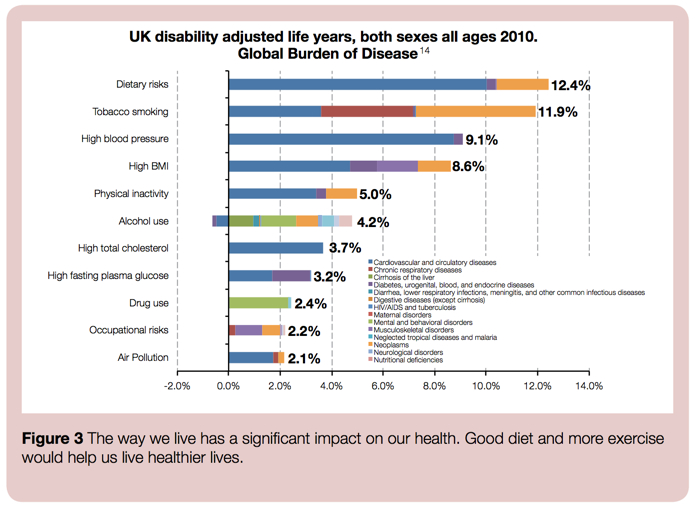
- physical inactivity is the fourth largest cause of disease and disability in the UK. [7]
Snowdon [1] notes:
If one looks at day-to-day exercise and occupational physical activity, it becomes clear that lifestyles have become more sedentary. The transition from manual labour to office work saw jobs in agriculture decline from eleven to two per cent of employment in the twentieth century while manufacturing jobs declined from 28 to 14 per cent of employment (Lindsay, 2003) [4]. Britons are walking less (from 255 miles per year in 1976 to 179 miles in 2010) and cycling less (from 51 miles per year in 1976 to 42 miles in 2010).
Only 18 per cent of adults report doing any moderate or vigorous physical activity at work while 63 per cent never climb stairs at work and 40 per cent spend no time walking at work (British Heart Foundation, 2012b: 58-59) [3]. Outside of work, 63 per cent report spending less than ten minutes a day walking and 53 per cent do no sports or exercise whatsoever (ibid.: 52-4). Add to this the ubiquity of labour-saving devices and it is clear that Britons today have less need, and fewer opportunities, for physical activity both in the workplace and at home."
Self-reported physical activity is increasing(Node #371615)The number of people who are self-reporting as meeting the government's recommendation of taking 30 minutes vigorous exercise five times a week rose from 26.5 per cent to 37.5 per cent between 1997 and 2012. [3]
Self-reported percentage of adults meeting the physical activity recommendations, by sex, UK countries 1997 to 2011

Source: British Heart Foundation / University of Oxford [1]
A minority of people are meeting the recommendations(Node #371616)
Although the number of people self-reporting as meeting the government's recommendations is rising, the total number remains a minority of the population.
The recommendations relate only to leisure activities(Node #371617)
The government recommendations, on which people are self-reporting, relate only to leisure activities – and other lifestyle factors (especially the increasingly sedentary patterns of behaviour) may be more significant in this context.
Calorie consumption(Node #352522)
Public Health England estimates that the average man in England is consuming around 300 calories a day more than they would need were they a healthy body weight.
Consuming too much sugar(Node #351718)Many people are eating more sugar than they should. Current intakes of sugar for all population groups exceed recommendations set by the Committee on Medical Aspects of Food Policy (COMA) for the UK in 1991 (which recommended that, on a population basis, no more than 10% of the average total energy intake should be consumed as sugar). Energy dense diets, such as those that are high in sugar, can lead to an excess calorie intake (which, if sustained, leads to weight gain and obesity).
Consuming more sugar-sweetened beverages(Node #348698) - Drinking just one regular soda a day is the equivalent of consuming over 221,000 sugar cubes over an average lifetime.
- Evidence shows that SSBs are major contributors to childhood obesity [19], [20], as well as to long-term weight-gain, type 2 diabetes, and cardiovascular disease [21], [22].
UK purchases of not-low calorie soft drinks are falling(Node #371569)Household purchases of soft drinks were 3.1 per cent lower in 2013 compared to 2010, a fall of 54 grams per person per week. Within this category, household purchases of ‘not low calorie soft drinks’ are on a downward trend since 2010 and fell by 23 per cent between 2010 and 2013 from 1139 to 878 grams per person per week.
UK purchases of soft drink (concentrated and unconcentrated), 1992–2013
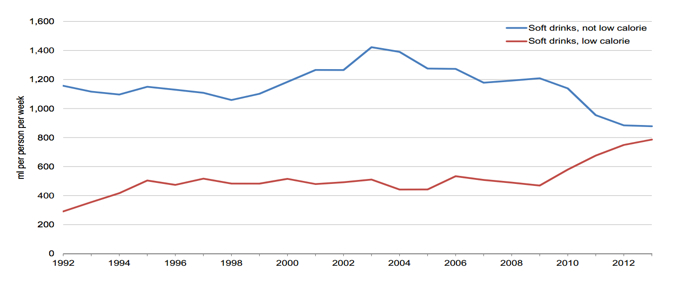
Source: DEFRA
- This was mirrored by an upward trend in ‘low calorie soft drinks’ with household purchases 36 per cent higher in the same period up from 579 to 786 grams per person per week.
Sugar(Node #368236)
Definitions of sugar vary. For the purposes of the PHE paper cited, the term ‘sugar’ includes all sugars outside the cellular structure in foods and drinks excluding those naturally present in dairy products. This includes sugar added to foods, plus the sugar in fruit juice and honey. It does not include the sugars naturally present in intact fruit and vegetables or dairy products.
Per capita sugar consumption has fallen by 16% since 1992(Node #371563)
Evidence suggests that per capita consumption of sugar, salt, fat and calories has been falling in Britain for decades. Per capita sugar consumption has fallen by 16 per cent since 1992 and per capita calorie consumption has fallen by 21 per cent since 1974.
WHO recommendations on sugar consumption(Node #400395)The World Health Organization (WHO) recommends (2015) that both adults and children limit their intake of added sugar to less than 10% of total daily calories; with conditional guidance to keep added sugar below 5% of daily calories (i.e. 6 teaspoons – 25 grams – per day for a 2,000-calorie diet).
- WHO recommends a reduced intake of free sugars throughout the lifecourse (strong recommendation).
- In both adults and children, WHO recommends reducing the intake of free sugars to less than 10% of total energy intake (strong recommendation).
- WHO suggests a further reduction of the intake of free sugars to below 5% of
total energy intake (conditional recommendation).
How sugar affects the brain(Node #372888)Eating sugar spikes dopamine levels and leaves a person craving more.
Choosing short-term pleasure over long-term health(Node #352517)
Disconnecting appetite from need and satiety (Node #352515)
Eating a price-led rather than a nutrition-led diet (Node #352518)
Intake around 5% higher than Estimated Average Requirement for adults(Node #371566)
Total energy intake from all food and drink is around 5 per cent higher than the Estimated Average Requirement for adult intakes.
Long term downward trend in total energy intake from all food & drink(Node #371565)Total energy intake per person was an average of 2192 kcal per person per day in 2012, 4.4 per cent lower than in 2010. This is a statistically significant downward trend that confirms the longer term downward trend already apparent since the mid 1960s.
Average energy intake from food and drink since 1940
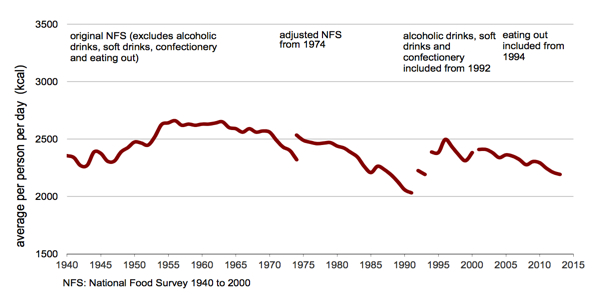
Source: DEFRA
Energy derived from household food and drink 2001-2013
Source: DEFRA
Measuring diet at a societal level is an inexact science(Node #371570)
Measuring diet at a societal level is an inexact science – as researchers generally have to rely on people keeping track of what they eat over a period of several days – and people may be inclined to under report their consumption patterns. Evidence suggests that people may throw away about 10-20% of the food they buy and underreport how much they eat by around 20–40%.
Type of calories consumed is significant (as well the quantity)(Node #371621)
Emerging research suggests that some foods and eating patterns may also make it easier to keep calories in check, while others may make people more likely to overeat. Many of the foods that help prevent disease also seem to help with weight control—foods like whole grains, vegetables, fruits, and nuts. And many of the foods that increase disease risk—chief among them, refined grains and sugary drinks—are also factors in weight gain.
Reluctance to talk about and address implications of own weight(Node #352389)
The weight of the population continues to rise despite media imagery of thin models encouraging a slim ideal that is far out of reach for most of the public. In this context, “Fat” remains an emotive and stigmatic subject – and often perceived as an insult – which makes it harder for people to acknowledge, confront and address their own obesity (and harder for others including health professionals to encourage them to do so too).
Dieting can make lean people fatter(Node #392052)
Dieting to lose weight in people who are in the healthy normal range of body weight is a strong and consistent predictor of future weight gain. [1]
Fat mass / fat-free mass depletion feedback signals are more effective(Node #392175)Lean people regain fat faster because their feedback signals in response to the depletion of both fat mass (i.e. adipostats) and fat-free mass (i.e. proteinstats) – through the modulation of energy intake and adaptive thermogenesis – are more effective than in individuals with overweight or obesity, thus resulting in a faster rate of fat recovery relative to recovery of lean tissue (i.e. preferential catch-up fat) [1], [2]
"In fact, it appears that lean people overshoot in terms of weight gain because the state of hyperphagia (in response to weight loss) appears to persist well beyond complete recovery of fat mass and interestingly until fat free mass is fully recovered (which may take months during which time fat gain continues)." [1]
Obesity alters neurocircuitry to increase susceptibility to overeating(Node #371333)
Obese people have alterations in dopamine neurocircuitry that may increase their susceptibility to opportunistic overeating while at the same time making food intake less rewarding, less goal directed and more habitual. Whether or not the observed neurocircuitry alterations pre-existed or occurred as a result of obesity development, they may perpetuate obesity given the omnipresence of palatable foods and their associated cues.
Strategies of some companies are fuelling the obesity crisis(Node #351042)
Some companies and industries are fuelling the obesity crisis, through a variety of strategies that prioritise profitability and corporate brand value over public health, and, in the process, externalise significant costs.
Production and marketing choices favour profit over diet optimisation(Node #368179)
Decisions made by many food and beverage companies tend to be shaped more by the immediate corporate financial interests of shareholders (and the associated interests of corporate officers) rather than the social goal of achieving optimal human diets; as reflected in, for example, the production and marketing a high volume of low-cost, highly processed foods that are rich in sugar, salt, and saturated fats.
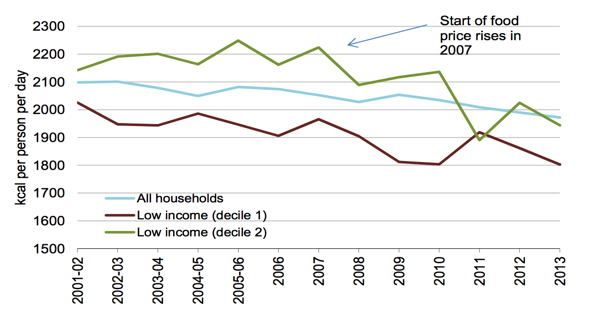
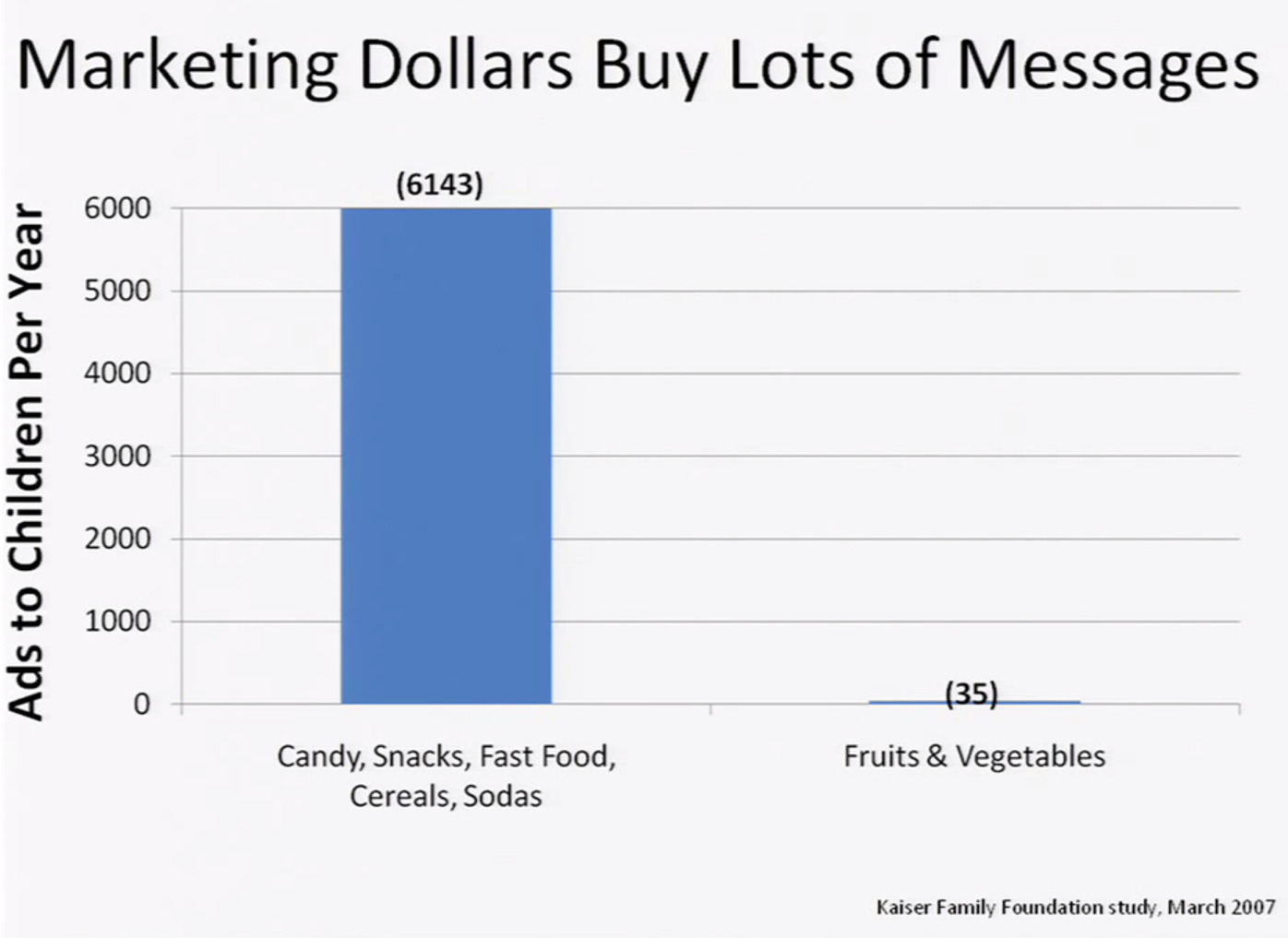
Advertising and marketing reinforce new eating patterns (Node #352388)Marketing and advertising instil and reinforce new cultural norms about what (e.g. fast food) and how to eat (e.g. snacking), and how much (e.g. larger portions) to eat.
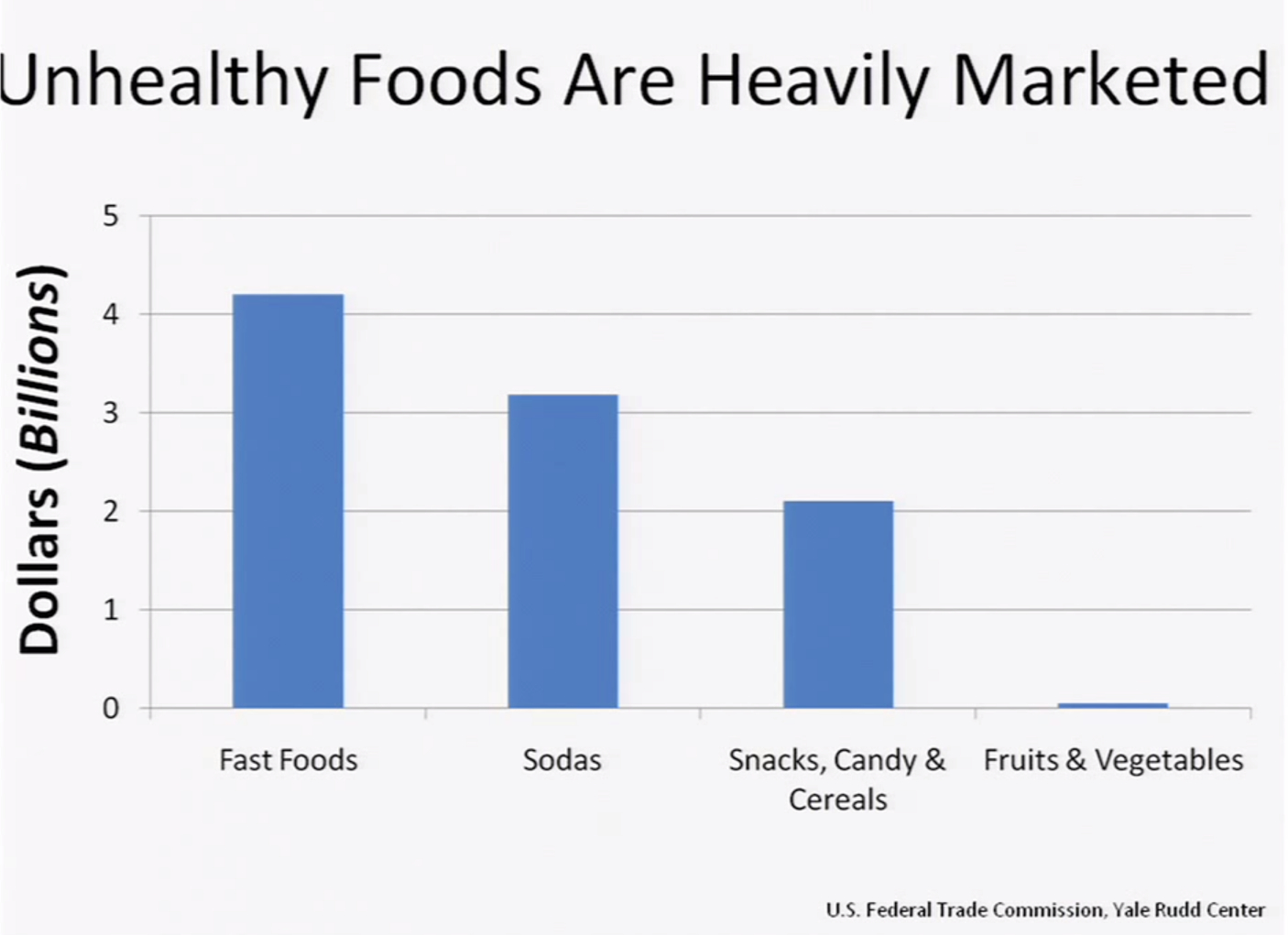

Sources: Scott Kahan, U.S. Federal Trade Commission, Yale Rudd Center, Kaiser Family Foundation
Targeting advertising at children(Node #368175)Advertising and other marketing approaches are targeted at children and other vulnerable groups.
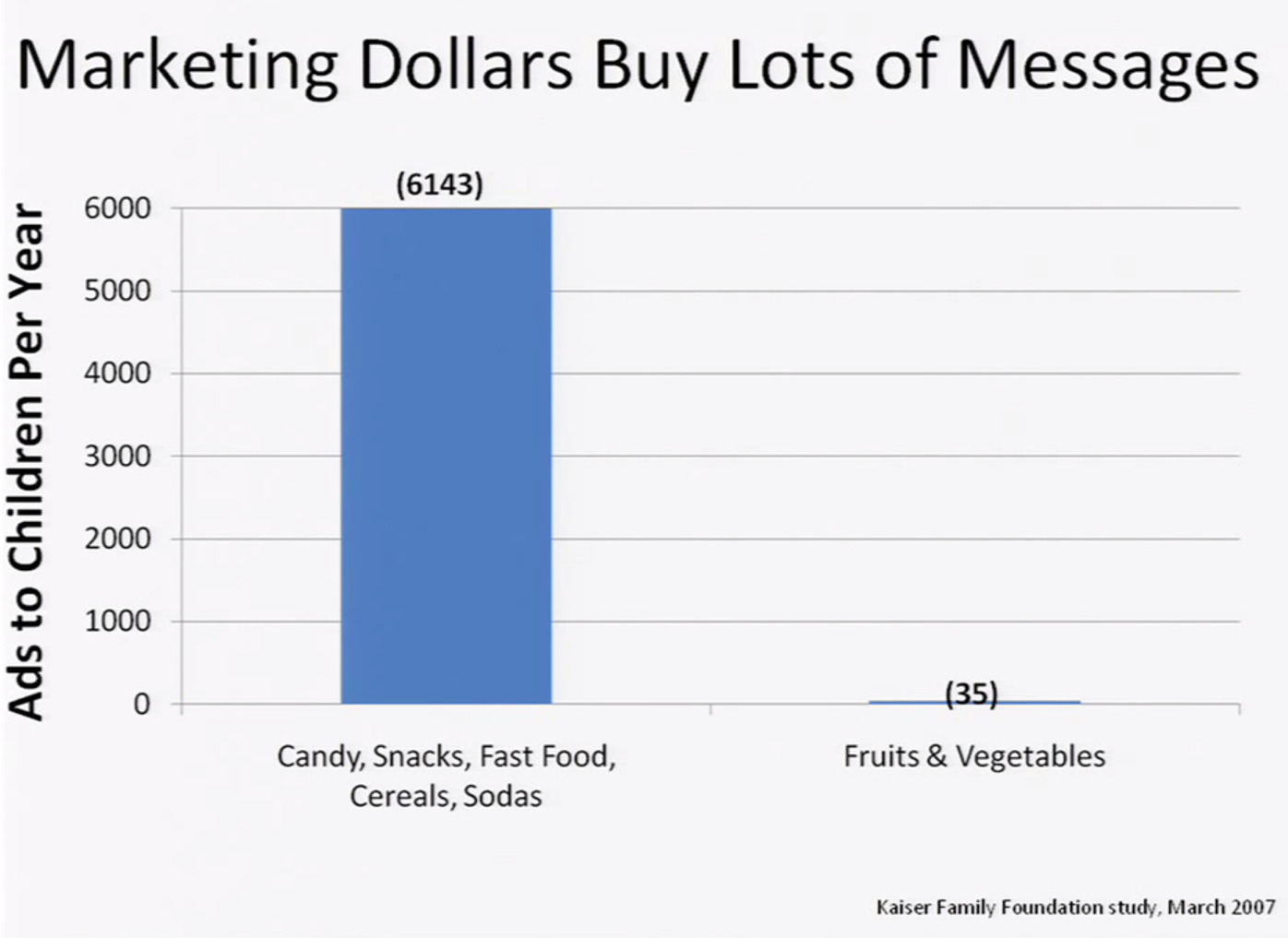

Sources: Scott Kahan, Kaiser Family Foundation
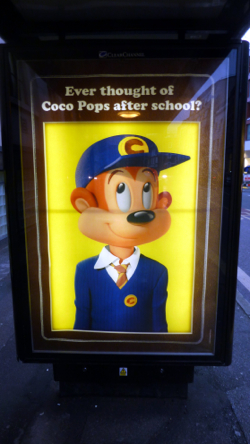
Impact of swapping away from sugary cereals(Node #371332)Swapping to plain cereals can cut your family's sugar intake by a quarter of a 1kg bag of sugar over 4-weeks.
Portions have grown larger(Node #370364)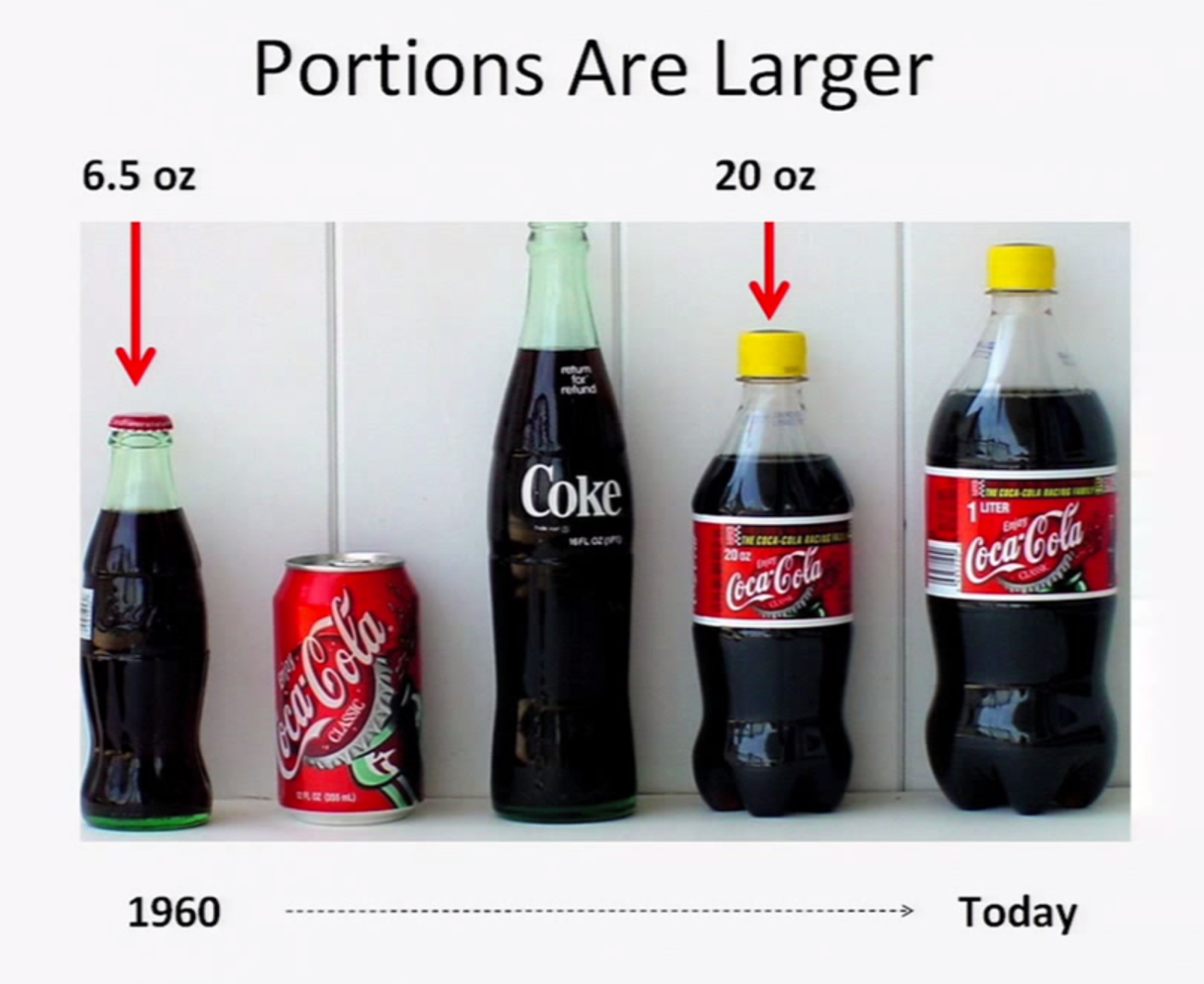
Source: Scott Kahan
Ready-to-eat food is more readily available(Node #370366)
Ready-to-eat food is increasingly available in industrial societies 24-hours a day and in places where food wasn't traditionally available (such as pharmacies and petrol stations), as well as via the growing number of fast food restaurants and coffee shops.
Fast food outlets – England(Node #371775)The concentration of fast food outlets and takeaways varies by local authority in England. The scatter plot shows a strong association between deprivation and the density of fast food outlets, with more deprived areas having more fast food outlets per 100,000 population. [1]
Growth in restaurants and dining out(Node #371727)The restaurant industry has almost doubled its share of every dollar spent on food in the United States over the last 60 years from 25% in 1955 to 47% today. Much of this growth reflects the expansion in fast food restaurants (a trend observed in other countries including the UK).
Unhealthier foods are engineered to be tastier(Node #370365)Food scientists have become adept at understanding how our brains respond to, and react to, and crave tastes, smells and textures, and have become adept at engineering and processing foods to take advantage of that – largely by adding lots of salt, sugar and fat – and to make these foods almost irresistible to our brains.
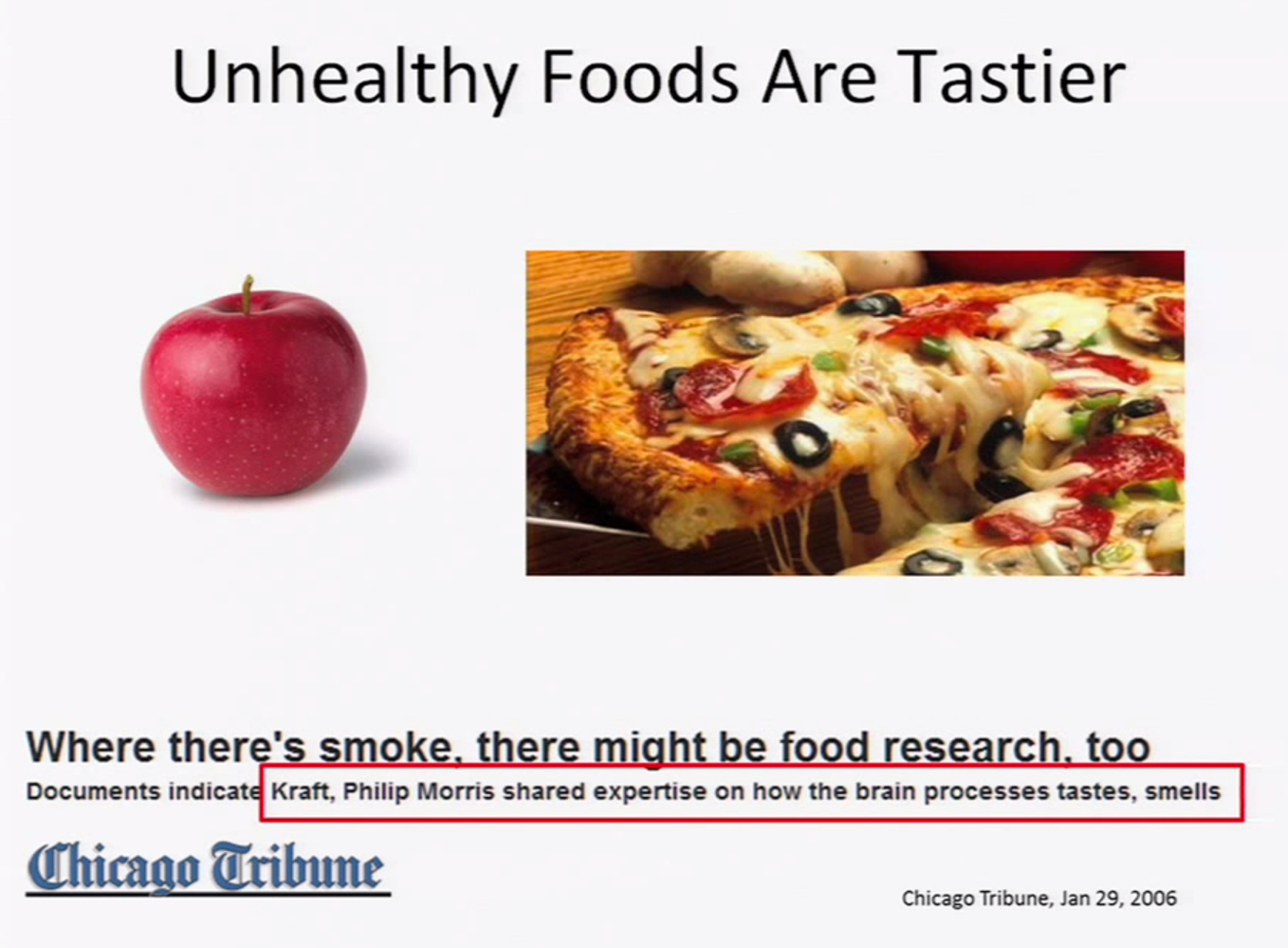
Sources: Scott Kahan, Chicago Tribune (2006)
- Although in theory minimal processing of foods can improve nutritional content, in practice most processing is done so to increase palatability, shelf-life, and transportability (and these processes tend to reduce nutritional quality). [2]
The addictiveness of sugar(Node #351120)Some companies are harnessing the addictiveness of sugar for commercial benefit and to the detriment of public health. Emerging science on the addictiveness and toxicity of sugar, especially when combined with the known addictive properties of caffeine found in many sugary beverages, points to a large-scale public health threat similar to addictiveness and harmful impacts of tobacco products.
Robert H. Lustig, MD, UCSF Professor of Pediatrics in the Division of Endocrinology, explores the damage caused by sugary foods. He argues that fructose (too much) and fiber (not enough) appear to be cornerstones of the obesity epidemic through their effects on insulin. Series: UCSF Mini Medical School for the Public [7/2009]
Fructose doesn't stimulate insulin or leptin or suppress ghrelin(Node #351139)
Fructose changes the way that the brain recognizes energy, so that the brain doesn't suppress appetite.
Fructose is 7 times more likely than glucose to form AGE's(Node #351137)
Fructose is 7 times more likely than glucose to form Advanced Glycation End-Products.
Fructose raises tryglicerides – a high sugar diet is a high fat diet(Node #351144)
Although fructose is a carbohydrate it is metabolized like a fat – a corollary of this is that a low fat diet isn't really low fat, because the fructose/sucrose doubles as fat.
HFCS products are sweeter and cheaper than cane sugar products(Node #366446)
Products with High Fructose Corn Syrup are sweeter and cheaper than products made with cane sugar.
Fructose is sweeter than glucose(Node #366444)
High fructose corn syrup is cheaper than cane sugar(Node #366445)
High fructose corn syrup is cheaper than sugar due to government farm bill corn subsidies in the US.
Unhealthy foods are cheaper and getting cheaper(Node #370363)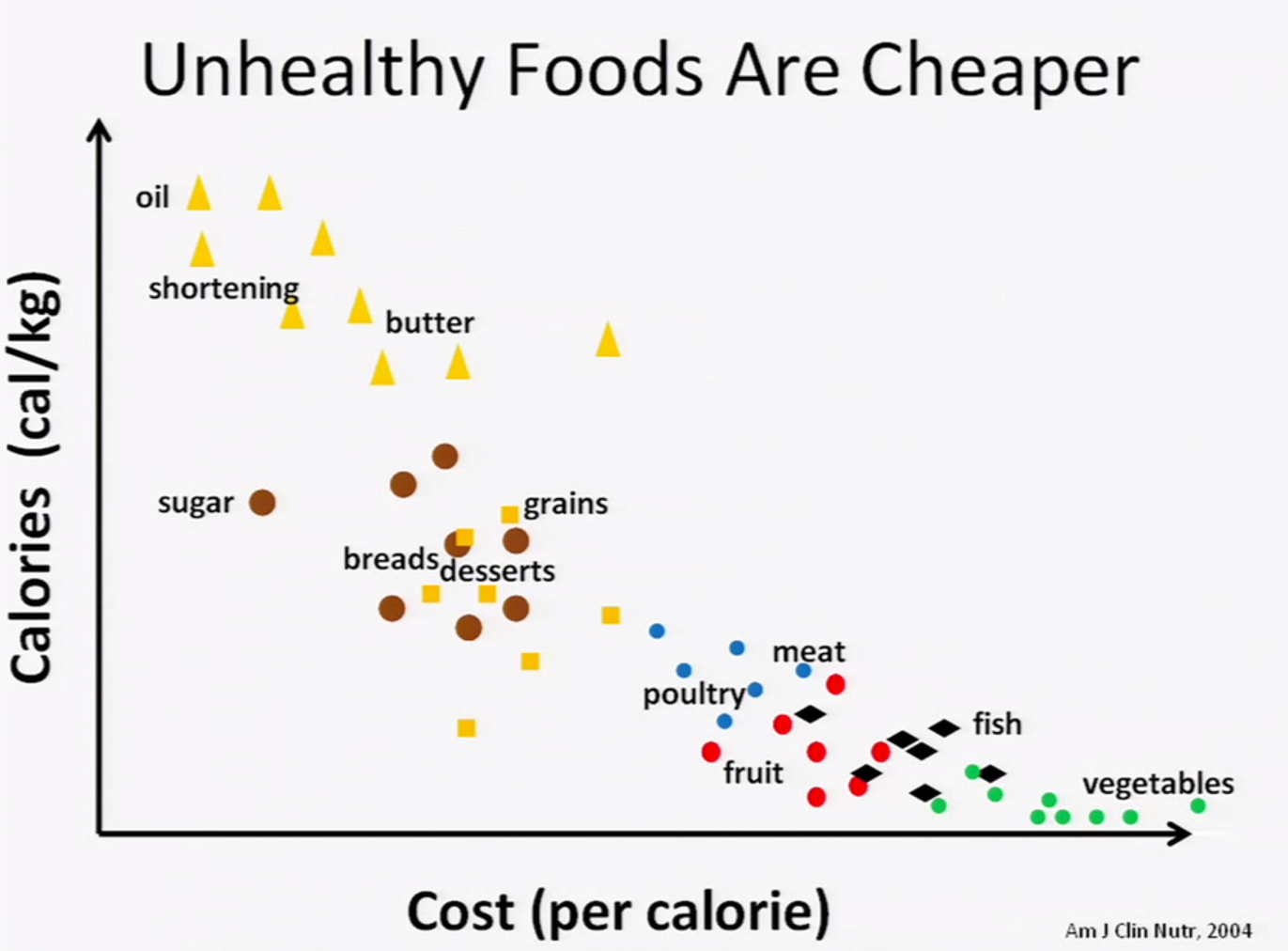
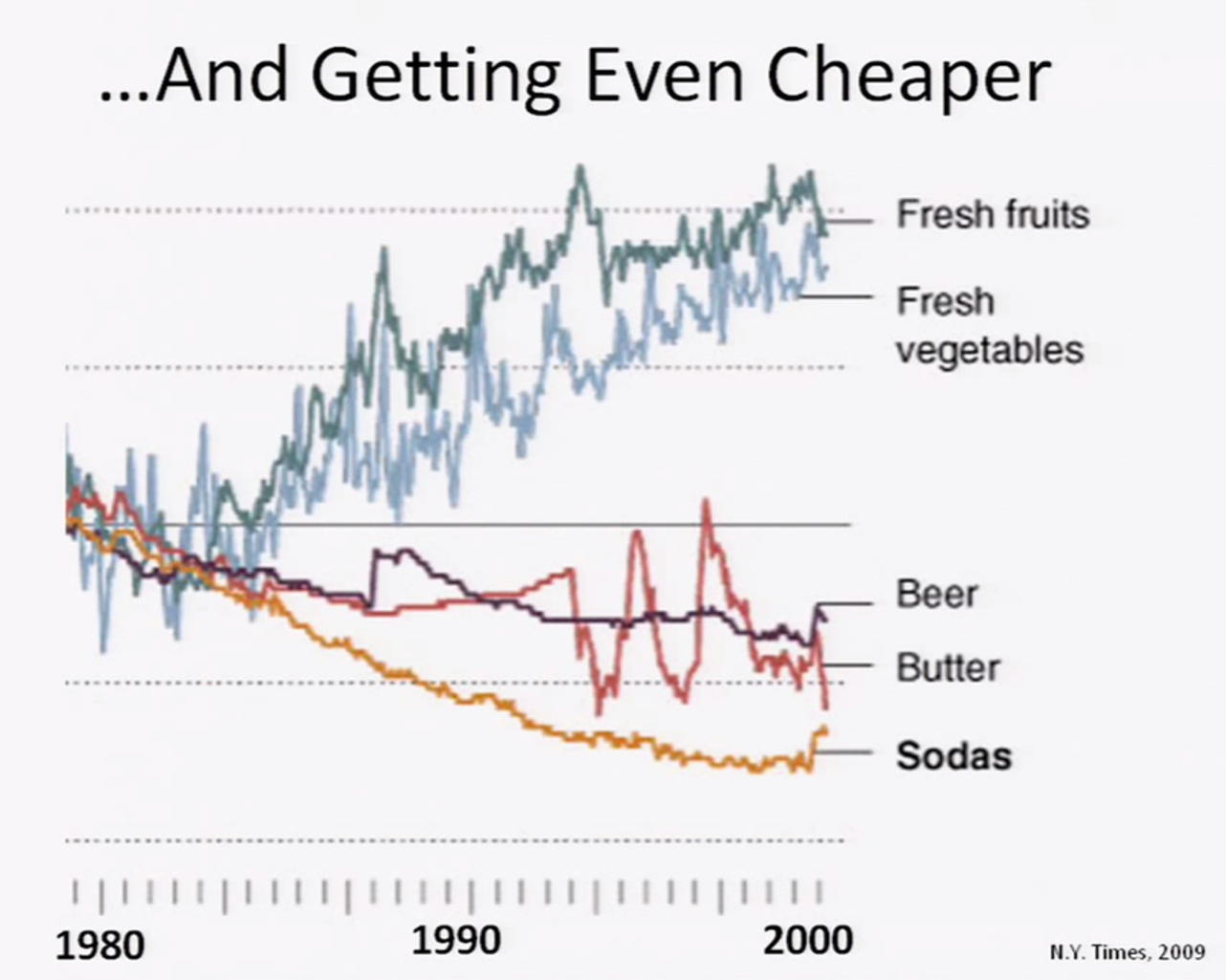
Sources: Scott Kahan, Am J Clin Nutr (2004), New York Times (2009)
Public health interventions are often resisted(Node #351043)Evidence suggests that, for example, some food and beverage companies are adopting similar tactics to those adopted earlier by the tobacco companies to avoid public health interventions (such as taxation and regulation) that might threaten their profits.
From Moodie et al. [6]:
- Transnational corporations are major drivers of non-communicable disease epidemics and profit from increased consumption of tobacco, alcohol, and ultra-processed food and drink (so-called unhealthy commodities).
- Alcohol and ultra-processed food and drink industries use similar strategies to the tobacco industry to undermine effective public health policies and programmes.
- Unhealthy commodity industries should have no role in the formation of national or international policy for non-communicable disease policy.
- Despite the common reliance on industry self-regulation and public–private partnerships to improve public health, there is no evidence to support their effectiveness or safety.
- In view of the present and predicted scale of non-communicable disease epidemics, the only evidence-based mechanisms that can prevent harm caused by unhealthy commodity industries are public regulation and market intervention
Adopting lessons from the Tobacco Playbook(Node #351113)The tobacco industry had a playbook, a script, that emphasized personal responsibility, paying scientists who delivered research that instilled doubt, criticizing the “junk” science that found harms associated with smoking, making self-regulatory pledges, lobbying with massive resources to stifle government action, introducing “safer” products, and simultaneously manipulating and denying both the addictive nature of their products and their marketing to children.
From Dorfman et al:
"Tobacco companies launched CSR campaigns to rehabilitate themselves with the public when their image had been tarnished [20]. Because the most comprehensive initiatives were introduced well after intense public outcry, however, their CSR efforts struggled to achieve their aims [42]. As soda denormalization is nascent, soda companies may enjoy benefits from CSR that Big Tobacco labored to accomplish. In addition to effectively preempting regulation and maintaining its favorable position with the public, the soda industry's CSR tactics may also entice today's young people to become brand-loyal lifetime consumers, an outcome that current social norms dictate Big Tobacco cannot explicitly seek.
Without sustained denormalization of soda, it will be harder for public health advocates to see why partnering with industry may further the companies' goals more than their own. While tobacco denormalization was facilitated by litigation, which used the discovery process to procure internal documents revealing the industry's duplicitous intent, it is possible to respond to the soda industry without a “smoking gun.”
For example, one instance of tobacco industry denormalization that did not rely on internal documents was the revelation that PM spent more on publicizing its charitable efforts than it spent on the charities itself, which exposed the cynical nature of Big Tobacco's CSR [114]. The Refresh Project's $20 million price tag, and the statements from company representatives, give public health advocates a similar opportunity to argue that this is marketing, not philanthropy [115].
Such criticism appeared in a Lancet editorial, which stated that the U.K.'s Change4Life should have avoided “ill-judged partnerships with companies that fuel obesity” [116]. Research on the health harms of sugary beverages can help advocates name these products as one of the “biggest culprits” [117] behind the obesity crisis.
Emerging science on the addictiveness [118] and toxicity [119] of sugar, especially when combined with the known addictive properties of caffeine found in many sugary beverages, should further heighten awareness of the product's public health threat similar to the understanding about the addictiveness of tobacco products.
Public health advocates must continue to monitor the CSR activities of soda companies, and remind the public and policymakers that, similar to Big Tobacco, soda industry CSR aims to position the companies, and their products, as socially acceptable rather than contributing to a social ill."
Shaping public understanding and scientific research(Node #371078)Well-resourced food companies are able to recruit leading nutritional scientist, experts and researchers to guide and justify product development, reformulation and health impact. Research suggests that studies funded by industry are 4- to 8-fold more likely to support conclusions favourable to the industry.
Successive governments have made counterproductive policy choices(Node #352399)
The growing prevalence of obesity in the UK is partly the result of well-intentioned but counterproductive policy choices made by successive governments over several decades.
Giving obesity a disproportionately low public health priority(Node #352558)The table below (via HOOP) [1] provides a summary of each of the public health issues, the prevalence of the issue in adults and children and young people as well as the direct NHS and indirect social and economic costs, (where data is available):
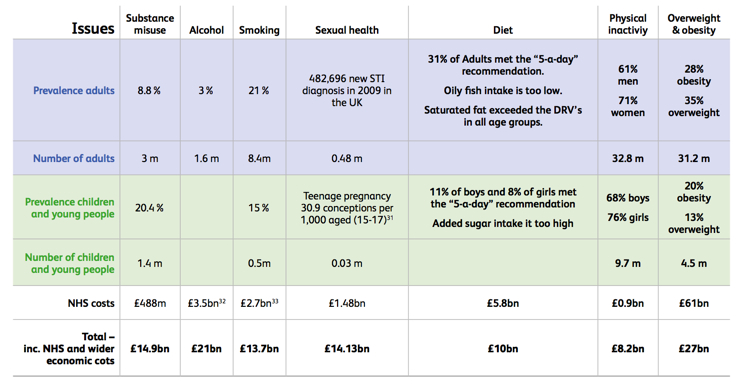
View full size>>
- Despite the higher direct and indirect costs, the allocation of public health funds by local authorities to help overweight and obese people to lose weight is significantly lower than the allocation for other public health issues.
- This is short sighted and this lack of action is the primary reason we are not seeing progress on tackling obesity.
- Why central government funding for weight management services is not available whilst £2bn worth of central government funding has been made available for substance misuse (in addition to already high local authority investment).
- Evidence seems to suggest that both central and local governments are either not aware of the disparity or they are simply not taking the issue of obesity seriously when compared to other public health issues.
- Given evidence that weight management services are cost effective local and central governments should be prioritising investments that provide a positive return.
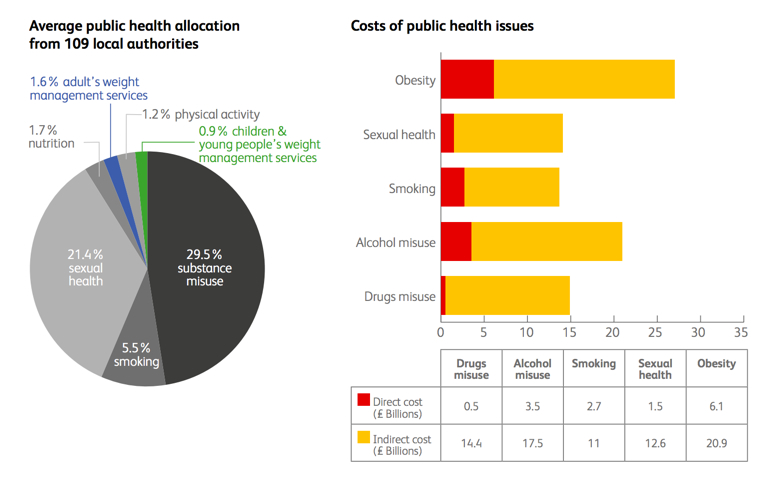
View full size>>
Inconsistent prioritisation of measures to protect population health(Node #352525)
Government patterns of interventions to protect the health of the population are inconsistent (e.g. interventions on smoking but not nutrition).
Paucity of investment in intervention measures(Node #366463)
The UK invests less than $1 billion a year in prevention activities such as weight-management programs and public health campaigns – i.e. around 1% of the social cost of obesity in the UK. More investment is required.
Weight management services in the UK are poorly developed(Node #352559)Although the prevalence of obesity in adults and in children in the UK is amongst the highest in the developed world, the multidisciplinary services necessary to manage patients with an established problem of excess weight and its clinical consequences are poorly developed within the UK. Some prevention and intervention strategies are provided in primary care, but secondary care and specialist services remain underdeveloped or unavailable to meet the need.
- Some prevention and intervention strategies are provided in primary care, but secondary care and specialist services remain underdeveloped or unavailable to meet the need.
Overseeing a decline in physical activity(Node #352531)
Successive governments have overseen a decline of physical activity (e.g. due to policies on transport, public spaces, and sports facilities).
Prioritising car use in retail and transport planning(Node #352532)
Subsidising the production of sugar and fat(Node #352528)
Governments are subsidising production of fat and sugar compared with micronutrient-rich foods.
EU Common Agricultural Policy(Node #370190)
The burden of diet-related disease has grown considerably since the introduction of the common agricultural policy (CAP) – the overarching framework used by EU member countries to form their own agricultural policies – which has subsidised the production of dairy products, red meat and sugar, and resulted in the systematic destruction of large quantities of fruit and vegetables.
Allowing an asymmetry of information on food, nutrition and health(Node #352527)Health education is overwhelmed by other marketing messages – generating an asymmetry of information flow and education on nutrition and health.

Sources: Scott Kahan, Kaiser Family Foundation
WHO's total budget is less than half the marketing budget of McDonalds(Node #366896)
McDonald’s and Coca-Cola’s marketing budgets are each twice the World Health Organization’s full-year budget.
Insufficient countervailing checks to oligopoly in food supply chains(Node #351336)The majority of what most people eat is driven increasingly by the production and distribution decisions of a few multinational food companies, whose oligopolistic interest are not necessarily aligned with the public health interest. Successive governments have failed to establish sufficient countervailing public policy measures to ensure that, where these interests are not aligned, the oligopolistic interests of the companies don't impact negatively on public health.
Background on the oligopoly in the global food system: [2]
- In the United States, the ten largest food companies control over half of all food sales [4] and worldwide this proportion is about 15% and rising.
- More than half of global soft drinks are produced by large multinational companies, mainly Coca-Cola and PepsiCo. [5] Three-fourths of world food sales involve processed foods, for which the largest manufacturers hold over a third of the global market.
- Big Food is a driving force behind the global rise in consumption of sugar-sweetened beverages (SSBs) and processed foods enriched in salt, sugar, and fat. [5]
Companies also deliver significant benefits(Node #368200)
Companies are source of food technology innovation(Node #368195)
Food companies are large employers(Node #368177)
Food companies are significant benefactors to political parties(Node #368178)
Food companies reduce the risk of undernutrition(Node #368194)
Advice to shift to low-fat diets may have been counterproductive(Node #371618)
Encouragement over the last 30 years to shift towards low-fat diets as the key to healthy weight and good health may have been misguided—as evidence suggests that low-fat diets don't make it easier to lose weight and don't appear to offer any special health benefits—and counterproductive as low-fat diets are often high in carbohydrates (especially from rapidly digested sources, such as white bread and white rice) which increase the risk of weight gain, diabetes, and heart disease.
What is obesity?(Node #352454)Obesity is a medical condition in which excess body fat has accumulated to the extent that it may result in increased health problems and reduced life expectancy. As central obesity (excess ectopic fat stored around major organs and abdomen) is the most dangerous form to health, waist measurement can be a key indicator of risk. Generally, men with a waist circumference of 94cm or more (and women of 80cm or more) are more likely to develop obesity-related health problems.
Illustration of obesity and waist circumference From left to right, as labeled in the original image, the "healthy" man has a 33 inch (84 cm) waist, the "overweight" man a 45 inch (114 cm) waist, and the "obese" man a 60 inch (152cm) waist. (image source) (image reference) Source: Report of the Dietary Guidelines Advisory Committee on the Dietary Guidelines for Americans, 2000. Infographic: FDA/Renée Gordon / Wikipedia
Body Mass Index (BMI) is also used as an indicator of healthy weight for height (although people who are very muscular can have a high BMI, without excess fat). For most adults:
- a BMI of 25 to 29.9 is considered overweight;
- a BMI of 30 to 39.9 is considered obese; and,
- a BMI of 40 or above is considered severely obese.
Older patients, in particular, may have a normal BMI while having a waist measurement which places them into the high risk category.
The Royal College of Physicians [4] notes that:
- Obesity is strongly heritable (60% of weight variance is attributed to heredity) yet currently known gene mutations and polymorphisms account for <5% of weight variability.
- Diagnosis by BMI requires measuring height and weight accurately; risk stratification in overweight and modest obesity requires measuring waist circumference and possibly the use of a clinical staging system (Edmonton Obesity Staging System (EOSS)).
- Prevention and long-term weight loss maintenance require sustained changes in diet and physical activity habits.
- Obesity is a major risk factor in diabetes (5 x), cancer (3 x the risk of colon cancer), and heart disease (2.5 x).
- Modest weight loss (~10 kg) helps to improve diabetes, improves quality of life and reduces morbidity.
- An energy deficit of only 100 calories per day predicts a 0.5 kg weight loss in a month.
- Cost-effective treatments in appropriate patients include weight loss programmes (commercial: e.g. WeightWatchers; GP delivered: eg Counterweight); pharmacotherapy (egorlistat); and bariatric surgery.
Assessing health risk and intervention(Node #370012)The latest guidance from the National Institute for Health and Care Excellence on the assessment of the health risk arising from obesity and associated interventions.
| BMI classification | Waist circumference |
| Low | High | Very high |
| Overweight | No increased risk | Increased risk | High risk |
| Obesity I | Increased risk | High risk | Very high risk |
- For men, waist circumference of less than 94 cm is low, 94–102 cm is high and more than 102 cm is very high.
- For women, waist circumference of less than 80 cm is low, 80–88 cm is high and more than 88 cm is very high.
| BMI classification | Waist circumference | Comorbidities present |
| Low | High | Very high |
| Overweight | 1 | 2 | 2 | 3 |
| Obesity I | 2 | 2 | 2 | 3 |
| Obesity II | 3 | 3 | 3 | 4 |
| Obesity III | 4 | 4 | 4 | 4 |
1 = General advice on healthy weight and lifestyle
2 = Diet and physical activity
3 = Diet and physical activity; consider drugs
4 = Diet and physical activity; consider drugs; consider surgery
Shortcomings of BMI?(Node #371489)
Although BMI is used widely as an indicator of obesity it has several shortcomings as an indicator.
Limited diagnostic accuracy(Node #371490)
The diagnostic accuracy of BMI to diagnose obesity is limited, particularly for individuals in the intermediate BMI ranges.
The BMI-mortality curve isn't constant for age(Node #371491)
BMI should be interpreted differently for different age groups.
The Obesity Paradox: higher BMI may not always be bad(Node #371492)
Research suggests that while being underweight and highly obese are both associated with increased mortality relative to the normal weight category, being overweight is not associated with excess mortality. Moreover, people with obesity who have preserved fitness and have no notable metabolic abnormalities have a very favourable prognosis; suggesting that improving fitness rather than weight loss per se should be emphasised in patients with overweight and class I obesity (BMI 30–35 kg/m2).
Statistics on Obesity, Physical Activity and Diet – England 2014(Node #371564)Statistics on Obesity, Physical Activity and Diet in England from the Health & Social Care Information Centre.
Obesity
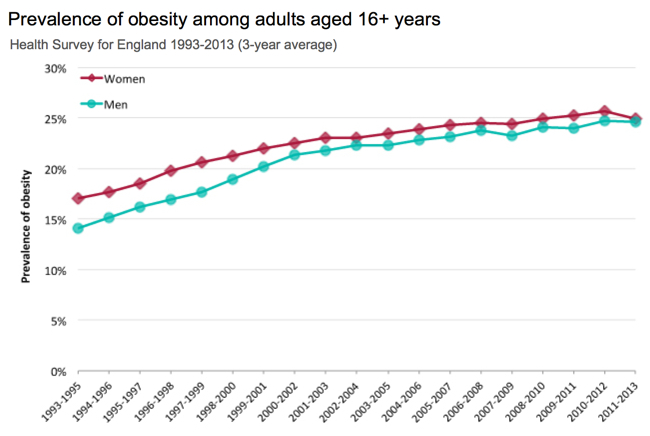
- The proportion of adults with a normal Body Mass Index (BMI) decreased between 1993 and 2012 from 41.0% to 32.1% among men and from 49.5% to 40.6% among women.
- There was a marked increase in the proportion of adults that were obese between 1993 and 2012 from 13.2% to 24.4% among men and from 16.4% to 25.1% among women.
- The proportion of adults that were overweight including obese increased between 1993 and 2012 from 57.6% to 66.6% among men and from 48.6% to 57.2% among women.
- The proportion of adults with a raised waist circumference increased from 20% to 34% among men and from 26% to 45% among women between 1993 and 2012.
- In Reception class in 2012/13, the proportion of obese children (9.3%) was lower than in 2011/12 (9.5%) and also lower than in 2006/07 (9.9%) (when data was first published).
- In Year 6 in 2012/13, the proportion of obese children (18.9%) was lower than in 2011/12 (19.2%) but higher than in 2006/07 (17.5%).
Physical activity In 2012
- 67% of men and 55% of women aged 16 and over met the new recommendations for aerobic activity. 26% of women and 19% of men were classed as inactive.
- 46% of men and 37% of women reported walking of at least moderate intensity for 10 minutes or more on at least one day in the last four weeks.
- 52% of men and 45% of women had taken part in sports/exercise at least once during the past four weeks.
Diet
- While overall purchases of fruit and vegetables reduced between 2009 and 2012, consumers spent 8.3% more on fresh and processed vegetables and 11.7% more on fresh and processed fruit.
- Total expenditure on household food and non-alcoholic drink rose by 4.3% in 2012 from the previous year and was 8.9% higher than in 2009. There have been significant upward trends in household expenditure on total fats and oils, butter, sugar and preserves, fruit and fruit juice, soft drinks and beverages.
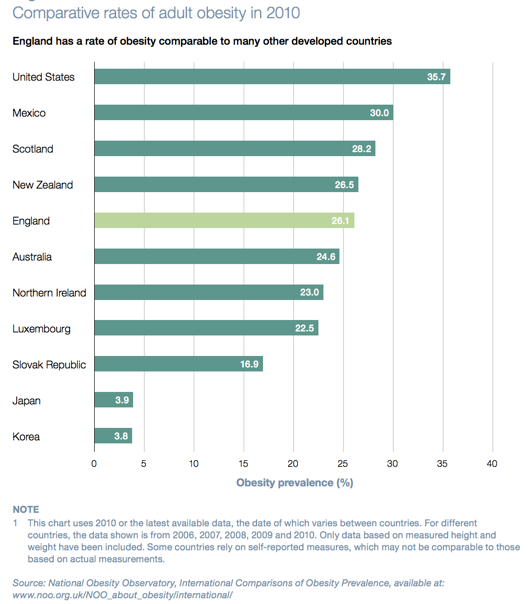
Impacts of obesity(Node #348688)Obesity presents a significant threat to the health of the UK population and a significant drain on the nation's financial resources. 24.9% of adults in England are obese—with a body mass index of over 30—62% of adults are either overweight or obese (with a BMI of over 25), and 32% of 10–11-year-olds are overweight or obese. The annual cost of obesity to the UK is estimated to be £27bn–£46bn [1], [2]; although international comparisons suggest that the true cost could be significantly higher.
Source: Public Health England – Obesity
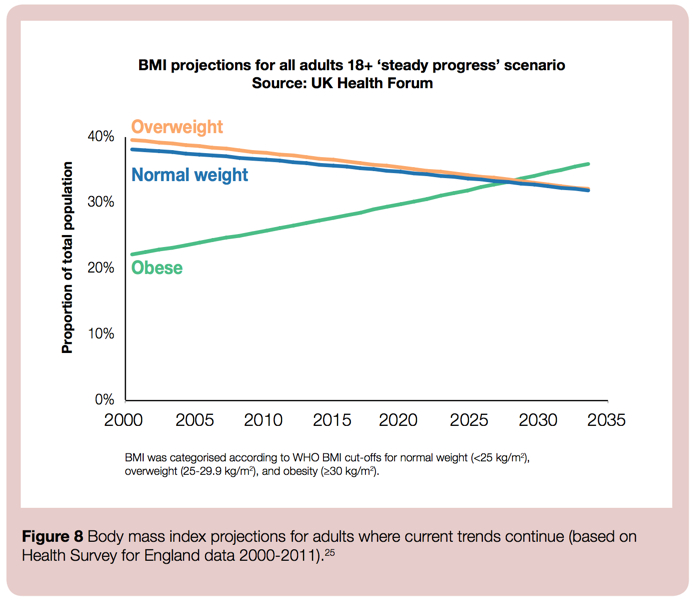
If the historic trends persist, one in three people will be obese by 2034 [6] (see chart below); although there are encouraging signs that the trend appears to have levelled off in children and may be levelling off among younger adults (reflecting, perhaps, the systemic progress being made in recent years). [8]
Nonetheless, the absolute level of obesity remains very high and England (along with the rest of the UK) ranks as one of the most obese nations in the world; there are no signs yet of a sustained decline, and (as obesity tends to increase with age) the UK's ageing population remains a concern.
A profound impact on the health of the population(Node #348776)Obesity is responsible for more than 9,000 premature deaths each year in England, reduces life expectancy on average by nine years, and is a major risk factor in wide range of serious health problems including Type 2 diabetes (5 x), cancer (3 x the risk of colon cancer), and heart disease (2.5 x).
Source: Public Health England [9]
Compared with a non-obese man, an obese man is:
- five times more likely to develop type 2 diabetes
- three times more likely to develop cancer of the colon
- more than two and a half times more likely to develop high blood pressure – a major risk factor for stroke and heart disease.
An obese woman, compared with a non-obese woman, is:
- almost thirteen times more likely to develop type 2 diabetes
- more than four times more likely to develop high blood pressure
- more than three times more likely to have a heart attack.
Risks of other diseases, including angina, gall bladder disease, liver disease, ovarian cancer, osteoarthritis and stroke, are also increased.
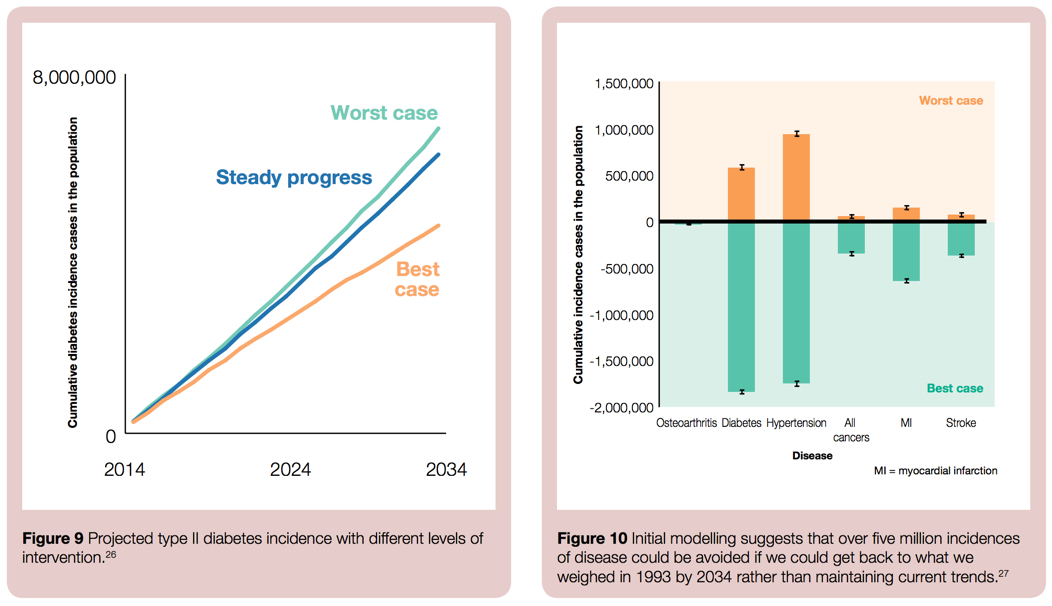
If current trends persist, one in three people will be obese by 2034 and one in ten will develop type II diabetes (Figure 9, below); whereas, reducing obesity back to 1993 levels, would avoid five million cases of disease (Figure 10, below).
Source: Public Health England [9]
- Around 58% of type 2 diabetes, 21% of heart disease and between 8% and 42% of certain cancers (endometrial, breast, and colon) are attributable to excess body fat.
- Obesity reduces life expectancy by an average 9 years and is responsible for 9,000 premature deaths a year in England.
- In addition, people who are obese can experience stigmatisation and bullying, which can lead to depression and low self-esteem. [1]
Increased risk of Type 2 diabetes (Node #352351)Obesity substantially raises the risk of Type 2 diabetes—with excess body fat estimated to underlie almost two-thirds of cases of diabetes in men and three quarters of cases in women—and people at risk of diabetes can cut their chances of getting diabetes by 60% if they lose between 5% and 7% of their body weight. Worldwide, the number of people with diabetes has tripled since 1985. [2]
Prevalence: Being overweight or obese is the main modifiable risk factor for type 2 diabetes. In England, obese adults are five times more likely to be diagnosed with diabetes than adults of a healthy weight. Currently 90% of adults with type 2 diabetes are overweight or obese. People with severe obesity are at greater risk of type 2 diabetes than obese people with a lower BMI.
Health impact: People with diabetes are at a greater risk of a range of chronic health conditions including cardiovascular disease, blindness, amputation, kidney disease and depression than people without diabetes. Diabetes leads to a two-fold excess risk for cardiovascular disease, and diabetic retinopathy is the leading cause of preventable sight loss among people of working age in England and Wales. Diabetes is a major cause of premature mortality with around 23,300 additional deaths in 2010-11 in England attributed to the disease.
Economic impact: It is estimated that in 2010-11 the cost of direct patient care (such as treatment, intervention and complications) for those living with type 2 diabetes in the UK was £8.8 billion and the indirect costs (such productivity loss due to increased death and illness and the need for informal care) were approximately £13 billion. Prescribing for diabetes accounted for 9.3% of the total cost of prescribing in England in 2012-13.
Type 2 diabetes
- The underlying disorder for type 2 diabetes is usually insulin insensitivity combined with a failure of pancreatic insulin secretion to compensate for increased glucose levels. The insulin insensitivity is usually evidenced by excess body weight or obesity, and exacerbated by over-eating and inactivity.
- It is commonly associated with raised blood pressure and a disturbance of blood lipid levels. The insulin deficiency is progressive over time, leading to a need for lifestyle change often combined with blood glucose lowering therapy.
- Factors which influence someone's risk of type 2 diabetes include: weight, waist circumference, age, physical activity and whether or not they have a family history of type 2 diabetes.
- Particular conditions can increase the risk of type 2 diabetes. These include: cardiovascular disease, hypertension, obesity, stroke, polycystic ovary syndrome, a history of gestational diabetes and mental health problems. In addition, people with learning disabilities and those attending accident and emergency, emergency medical admissions units, vascular and renal surgery units and ophthalmology departments may be at high risk.
- In addition to these individual risk factors, people from certain communities and population groups are particularly at risk. This includes people of South Asian, African-Caribbean, black African and Chinese descent and those from lower socioeconomic groups.
Metabolic Syndrome
- Metabolic syndrome is a combination of disorders including high blood glucose, high blood pressure and high cholesterol and triglyderide levels, that is more common in obese individuals and is associated with significant risks of coronary heart disease and Type 2 diabetes. There is also a greater risk of dyslipidemia (for example, high total cholesterol or high levels of triglycerides), which also contributes to the risk of circulatory disease by speeding up atherosclerosis (fatty changes to the linings of the arteries).
Diabesity(Node #387636)
Diabetes caused by overweight or obesity (and synonymous with the usual form of type 2 diabetes). UCLA started a Diabesity Research Program in 1998. [4]
Increased risk of several cancers(Node #351181)The risk of several cancers is higher in obese people, including endometrial, breast and colon cancers. BMI is associated with cancer risk, with substantial population-level effects (although the heterogeneity in the effects suggests that different mechanisms are associated with different cancer sites and different patient subgroups).
- The International Agency for Research on Cancer (IARC) has found that around 7,000 male and 13,000 female cancer cases in the UK each year could be attributed to obesity –and that over four in 10 cancers in the UK could be prevented through lifestyle changes that encourage healthy eating and exercise. [5]
- Research has suggested that body-mass index (BMI) is an important predictor of cancer risk, 2 and a Norwegian cohort study reported associations with several cancer sites, including the thyroid 3 and ovaries; 4 and the UK Million Women Study showed associations between BMI and ten of 17 sites investigated.5
- Two large reviews brought these and many smaller studies together.6, 7 In a meta-analysis of 221 datasets, strong associations were recorded between BMI and cancers of the oesophagus, thyroid, colon, kidneys, endometrium, and gallbladder, and weaker associations were shown for several other sites. 7
- Increased BMI was negatively associated with lung cancer.
Increased risk of heart disease(Node #352349)
Raised BMI increases the risk of hypertension (high blood pressure), which is itself a risk factor for coronary heart disease and stroke and can contribute to other conditions such as renal failure. The risk of coronary heart disease (including heart attacks and heart failure) and stroke are both substantially increased. Risks of deep vein thrombosis and pulmonary embolism are also increased.
Increased risk of musculoskeletal disability(Node #352344)Raised body weight puts strain on the body's joints, especially the knees, increasing the risk of osteoarthritis (degeneration of cartilage and underlying bone within a joint). There is also an increased risk of low back pain.
- There is a two-way relationship between obesity and disability in adults.
- Obesity is associated with the four most prevalent disabling conditions in the UK: arthritis, back pain, mental health disorders and learning disabilities.
- One third of obese adults in England have a limiting long term illness or disability compared to a quarter of adults in the general population.
- The prevalence of obesity-related disabilities among adults is increasing.
- Adults with disabilities have higher rates of obesity than adults without disabilities.
- For those adults who are disabled and obese, social and health inequalities relating to both conditions may be compounded. This can lead to socioeconomic disadvantage and discrimination.
- The combination of rising obesity and disability has significant implications for health and social care services in England.Obesity may lead to disability as a consequence of increased body weight, associated co-morbidities, environmental factors, or a combination of these.
- Obesity places mechanical stress on joints, increasing the risk of back pain and osteoarthritis which may in turn limit mobility. Some obese people may face difficulties in performing tasks such as walking, climbing steps, driving or dressing. This in turn can lead to physical inactivity, pain and discomfort, functional limitations and mental distress.
- Older people who are obese are at particular risk of joint pain and arthritis and may be less motivated to engage in physical activity if they are concerned about falls and bone fractures.
- Among people with severe obesity, limitations in mobility-related activities have been reported to be between five and nine times greater than for healthy weight subjects.
- A recent UK cohort study of adults with severe obesity found that the prevalence of self-reported disability was strongly associated with BMI, age, the presence of type 2 diabetes, metabolic syndrome and clinical depression.
Increased risk of gastrointestinal disease(Node #352356)
Obesity is associated with: increased risk of gastro-oesophageal reflux and increased risk of gall stones.
Increased risk of non-alcoholic fatty liver disease(Node #352355)The term ‘non-alcoholic fatty liver disease’ (NAFLD) refers to a range of conditions resulting from the accumulation of fat in cells inside the liver. It is one of the commonest forms of liver disease in the UK. If left untreated, it may progress to severe forms such as non-alcoholic steatohepatitis (NASH), fibrosis and cirrhosis. It has also been linked to liver cancer.
- Obesity is an important risk factor for the condition: over 66% of overweight people, and over 90% of obese individuals are at risk of NAFLD.
- As levels of obesity have risen, so has the prevalence of NAFLD. There is a lack of high quality data related to the prevalence of NAFLD in the UK. This is due to a number of factors including variations in diagnostic criteria, the invasive nature of diagnosis, and the lack of symptoms in people with mild forms of the condition.
- Approaches to tackling the condition focus on weight reduction through a combination of diet and physical activity, but there is no specific evidence-based treatment for NAFLD.
- Scientific understanding of the condition is limited, and there is a lack of high quality data on it. The impact of rising obesity levels on the prevalence and severity of NAFLD is not known, nor are the natural history or optimal management of the condition. There is a lack of scientific consensus on just how significant a threat to health NAFLD presents. In order to explore these issues in more detail we held an initial expert workshop in October 2013, and are continuing to develop this work in PHE and with external partners.
- Improvements in outcomes from NAFLD will require better data collection through primary and secondary care, death certification, and transplant registers, as well as research into the causes and treatment of the condition.
Increased risk of psychological and social problems(Node #352357)There are bi-directional associations between mental health problems and obesity, with levels of obesity, gender, age and socioeconomic status being key risk factors. Overweight and obese people can suffer from stress, low self-esteem, social disadvantage, depression and reduced libido.
- The mental health of women is more closely affected by overweight and obesity than that of men.
- There is strong evidence to suggest an association between obesity and poor mental health in teenagers and adults. This evidence is weaker for younger children.
- The perception of being obese appears to be more predictive of mental disorders than actual obesity in both adults and children (although the relationships between actual body weight, self-perception of weight and weight stigmatisation are complex and vary across cultures, age and ethnic groups).
- Weight stigma increases vulnerability to depression, low self-esteem, poor body image, maladaptive eating behaviours and exercise avoidance.
- There is an urgent need for evaluations of weight management interventions, both in terms of weight loss and psychological benefits.
- Intervention strategies should consider both the physical and mental health of patients. It has been recommended that care providers should monitor the weight of depressive patients and, similarly, in overweight or obese patients, mood should be monitored. This awareness could lead to prevention, early detection, and co-treatment for people at risk, ultimately reducing the burden of both conditions.
Blaming people living with obesity can be counterproductive(Node #391400)Blaming people living with obesity creates counterproductive tension between prevention and clinical care.
Increased risk of reproductive and urological problems(Node #352353)
Obesity is associated with greater risk of stress incontinence in women. Obese women are at greater risk of menstrual abnormalities, polycystic ovarian syndrome and infertility. Obese men are at higher risk of erectile dysfunction. Maternal obesity is associated with health risks for both the mother and the child and after pregnancy.
Increased risk of sleep apnoea and asthma(Node #352354)
Overweight and obese people are at increased risk of sleep apnoea (interruptions to breathing while asleep) and other respiratory problems such as asthma.
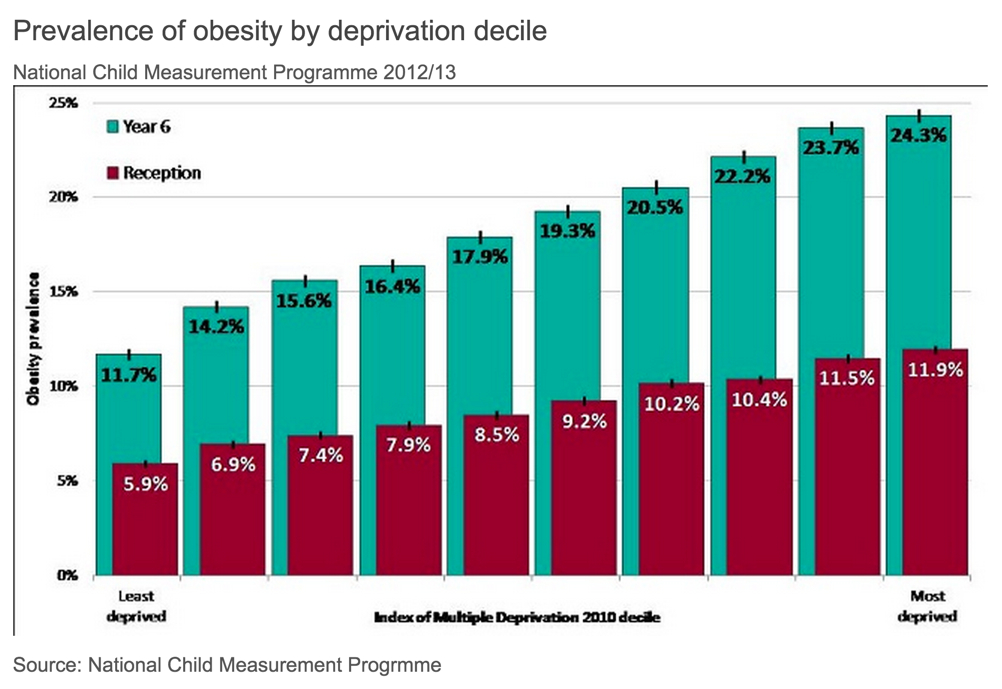
Inequality of impact(Node #351674)Although obesity occurs across all population groups, it impacts disproportionately on the socially and economically disadvantaged and some ethnic minorities. [8]
More Details – PHE Obesity >>
- Obesity is related to social disadvantage among adults [6], [8] and children [7], [8].
- It is also linked to ethnicity: it is most prevalent among African-Caribbean and Irishmen and least prevalent among Chinese women [7], [8].
Individual tragedy(Node #400252)Systemic problems like obesity involve many individual tragedies that touch many families' lives; some become symbolic of the national challenge but most are hidden in private pain and grief.
Life expectancy at birth has increased over the last 30 years(Node #371548)Life expectancy at birth, UK (1980-1982 to 2011-2013)
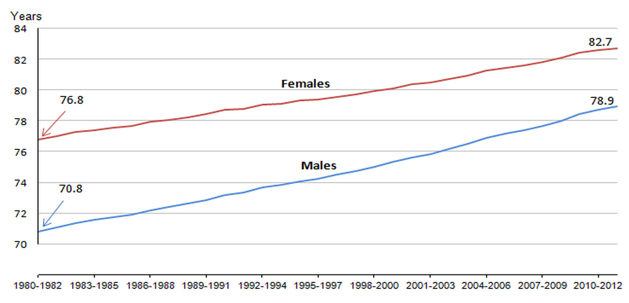
Source: ONS
The health consequences of rising obesity are not clear(Node #371553)
Although the incidence of overweight and obesity are increasing, the health consequences of the increasing incidence are not clear.
Body fat's role in excess mortality and morbidity remains uncertain(Node #371554)
A potentially unsustainable financial burden on the health system(Node #348767)The range of obesity's impacts makes accurate economic analysis challenging; however, a November 2014 study from the McKinsey Global Institute placed the annual economic impact on the UK at around $73bn (£46bn). Earlier analysis and modelling for the 2007 Foresight Report suggested a cost to the NHS of around £4.2bn annually to treat people with health problems related to elevated BMI and a total wider cost to the economy of around £15.8bn (rising to £27bn by 2015 and £49.9bn by 2050).
Simon Stevens, Chief Executive of NHS England warned in September 2014 of the need to get serious about obesity or bankrupt the NHS (with the cost of treating the health consequences of obesity escalating as the prevalence of obesity spreads in the population):
Obesity is the new smoking, and it represents a slow-motion car crash in terms of avoidable illness and rising health care costs... If as a nation we keep piling on the pounds around the waistline, we’ll be piling on the pounds in terms of future taxes needed just to keep the NHS afloat. [13]
The McKinsey Global Institute analysis [11] found that obesity generated an economic loss in the UK of more than $70 billion a year in 2012, or 3.0 percent of GDP (see below); the second biggest impact – within the analysis as defined (covering the loss of productive life, direct health-care costs, and investment to mitigate the cost) – of 14 human generated burdens:
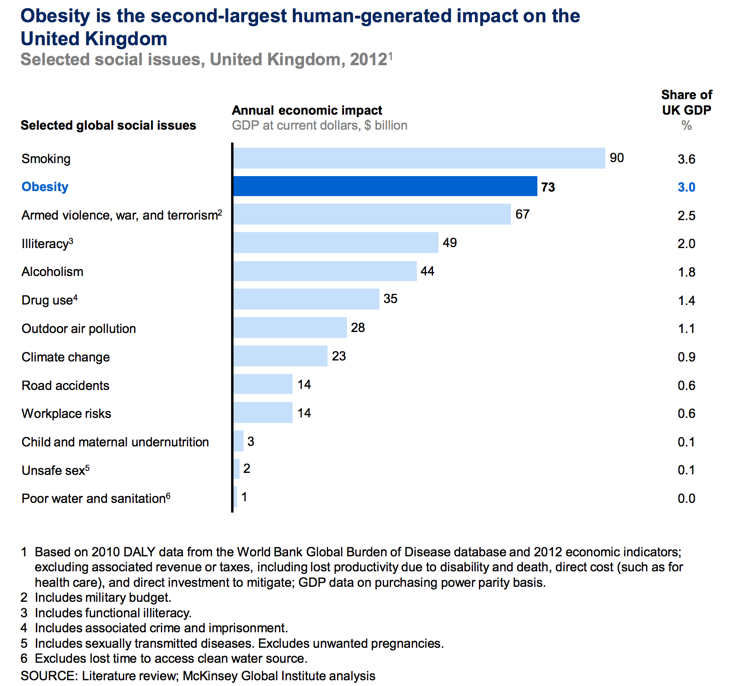
Source: McKinsey Global Institute
A 2010 review by the National Obesity Observatory of previous economic analyses of the burden of obesity in the UK noted: [2]
- Estimates of the direct NHS costs of treating overweight and obesity, and related morbidity in England have ranged from £479.3m in 1998 [4] to £4.2bn in 2007. [1]
- Estimates of the indirect costs (those costs arising from the impact of obesity on the wider economy such as loss of productivity) from these studies ranged between £2.6bn [4] and £15.8 billion.[1] Modelled projections suggest that indirect costs could be as much as £27bn by 2015. In 2006/07, obesity and obesity-related illness was estimated to have cost £148 million in inpatient stays in England. [10]
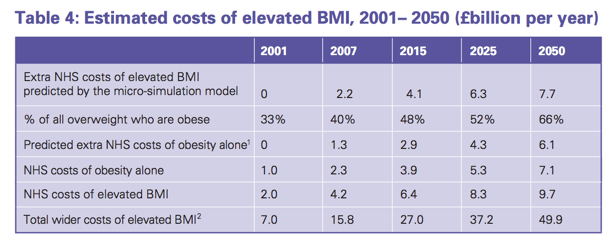
Source: Foresight Report, 2007
- Premature deaths attributable to obesity lead to the annual loss of around 45,000 years of working life. Sickness absence attributable to obesity is estimated at between 15.5 million and 16 million days per year.Obese people are much less likely to be in employment than those of healthy weight, with associated welfare costs estimated at between £1 billion and £6 billion. The total cost to the economy of being overweight or obese has been estimated as some £16 billion in 2007, rising to £50 billion per year by 2050 if left unchecked.
- It is estimated that 23% of spending on all drugs is attributable to overweight and obesity. The minimum annual cost of any drug prescriptions at BMI 20 rose from £50.71 for men and £62.59 for women by £5.27 and £4.20, respectively, for each unit increase in BMI to a BMI of 25.3 Increases for each BMI unit were greater to BMI 30, and greater still, £8.27 (men) and £4.95 (women), to BMI 40.
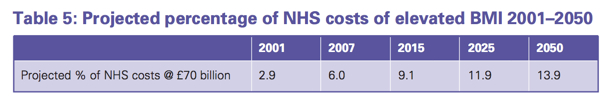
Source: Foresight Report, 2007
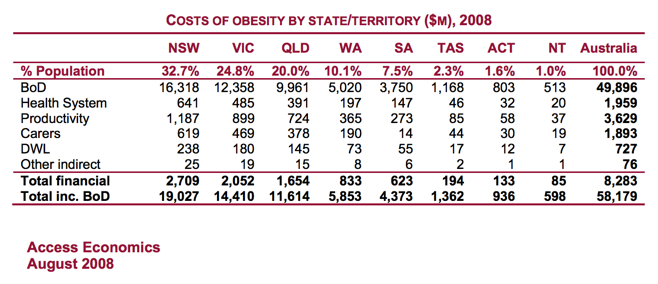
Financial cost of obesity – international comparisons(Node #370359) Financial cost of obesity – Australia(Node #362029)The overall annual cost of obesity to Australian society and governments was estimated to be $58.2 billion in 2008 – which, when adjusted for relative population, suggests that the actual overall annual cost of obesity to the UK may closer to £100m per year.
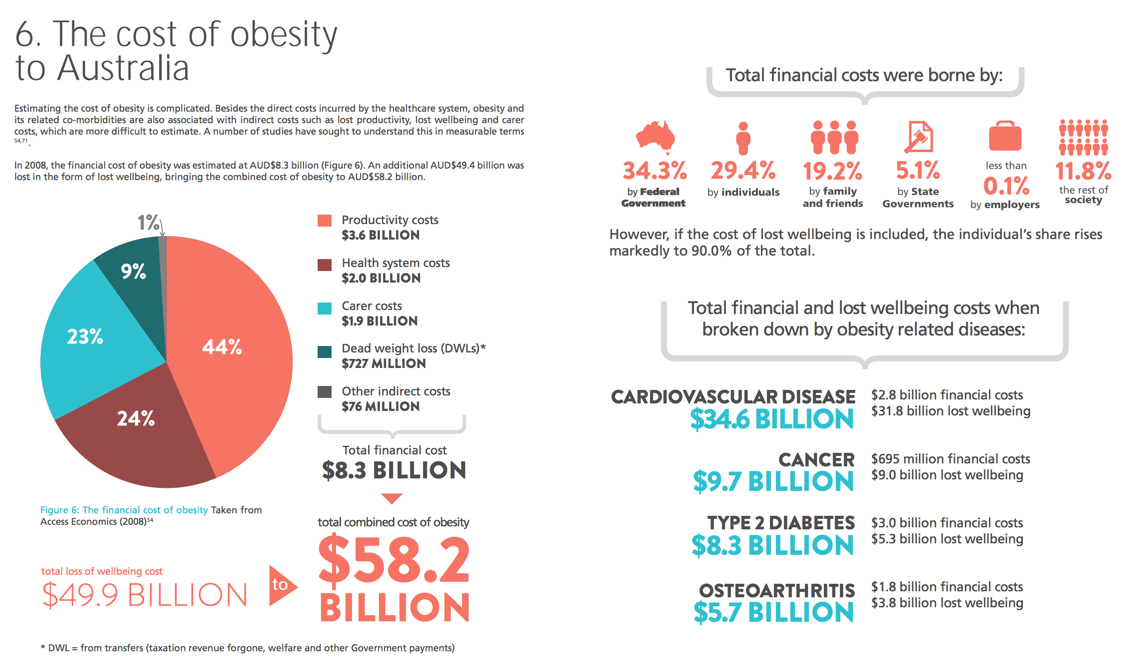
- The total direct financial cost of obesity for the Australian community was estimated to be $8.3 billion in 2008. Of these costs, the Australian Government bears over one-third (34.3% or $2.8 billion per annum), and state governments 5.1%.
- This estimate includes productivity costs of $3.6 billion (44%), including short- and long-term employment impacts, as well as direct financial costs to the Australian health system of $2 billion (24%) and carer costs of $1.9 billion (23%).
- The net cost of lost wellbeing (the dollar value of the burden of disease, netting out financial costs borne by individuals) was valued at $49.9 billion.
Financial cost of obesity – USA(Node #362031)Analysis [6] prepared for The Fiscal Times by Scott Kahan—director of the National Center for Weight & Wellness at George Washington University—puts the total national cost of obesity (including direct medical and non-medical services, decreased worker productivity, disability and premature death) at $305.1bn annually. Including the intangible costs associated with pain and suffering from obesity and obesity-associated conditions would add at least a further $300bn a year (Society of Actuaries).
- Direct medical costs (including counselling, outpatient and hospital visits, a range of bariatric surgical procedures, new treatment, nursing home care, rehabilitation and hospice) account for $190 billion of the annual costs. [5]
- Non-medical costs (including health education and behavioural change) add $50 billion per year.
- Absenteeism and sub-par productivity in the workplace costs an additional $65.1 billion a year.
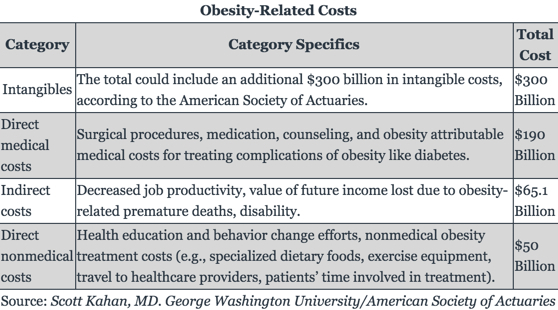
Earlier Analysis of the Economic Impact of Obesity on the US
- In 2010, the nonpartisan Congressional Budget Office reported that nearly 20 percent of the increase in U.S. health care spending (from 1987-2007) was caused by obesity.
- Annual health costs related to obesity in the U.S. is nearly $200 billion, and nearly 21 percent of medical costs in the U.S. can be attributed to obesity.
- Researchers estimate that if obesity trends continue, obesity related medical costs, alone, could rise by $43 to $66 billion each year in the United States by 2030.
- Per capita medical spending is $2,741 higher for people with obesity than for normal weight individuals.
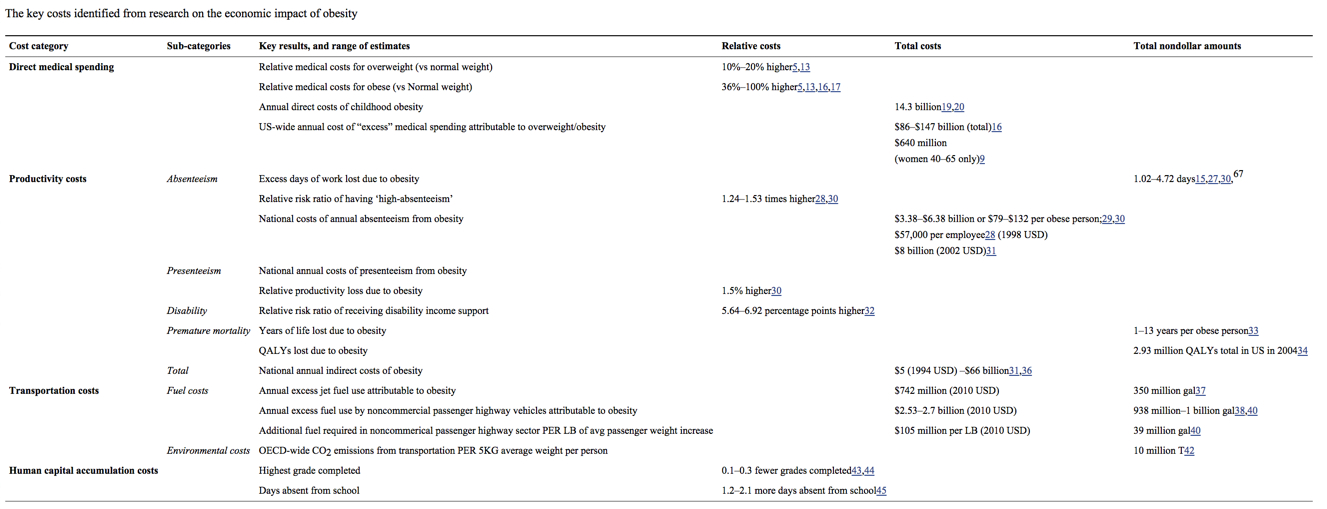
View full size >>
Obesity's Impact on the US Workforce
- Full-time workers in the U.S. who are overweight or obese and have other chronic health conditions miss an estimated 450 million additional days of work each year compared with healthy workers-- resulting in an estimated cost of more than $153 billion in lost productivity annually, according to a 2011 Gallup Poll.
- Medical expenses for obese employees are 42% than for a person with a healthy weight, according to the Centers for Disease Control.
What costs should be included in the financial analysis?(Node #366990)What cost factors should be included in the assessment of the overall financial impact of obesity on the UK economy?
Direct healthcare costs of obesity(Node #362119)
The direct costs of obesity are those that result from outpatient and inpatient health services (including surgery), laboratory and radiological tests, and drug therapy. [1]
Hospital Inpatient Visits(Node #362116)
Hospital Outpatient Visits(Node #362117)
Obesity Drug Costs(Node #362118)
Obesity Research Costs(Node #362127)
Indirect financial costs of obesity(Node #362121)
The indirect costs of obesity are the resources forgone as a result of an obesity-related health condition. [1]
Lost productivity(Node #352311)Obesity has as a serious impact on UK economic development – constraining economic productivity and increasing business costs – affecting individuals’ ability to get and hold down work, their self-esteem and their underlying mental health.
Absenteeism(Node #362122)
Obese employees miss more days from work due to short-term absences and long-term disability, than nonobese employees. [2]
Early retirement(Node #362124)
Obese employees are more likely, in general, to retire early than non-obese employees.
Human capital accumulation costs(Node #362140)
Days absent from school(Node #362141)
Highest grade completed(Node #362142)
Premature mortality(Node #362125)
Premature death is more likely, in general, among obese employees than non-obese employees.
QALYs lost due to obesity(Node #362139)
Years of life lost due to obesity(Node #362138)
Presenteeism(Node #362123)
Obese employees are more likely, in general, to work at less than full capacity than non-obese employees.
Costs of carers(Node #362128)
Lost taxation(Node #362130)
Transportation costs(Node #362131)
Environmental costs(Node #362132)
OECD-wide CO2 emissions from transportation(Node #362137)
OECD-wide CO2 emissions from transportation PER 5KG average weight per person
Fuel costs(Node #362133)
Additional fuel required in noncommerical passenger highway sector(Node #362136)
Additional fuel required in noncommerical passenger highway sector PER LB of avg passenger weight increase.
Annual excess fuel use by noncommercial passenger highway vehicles(Node #362135)
Annual excess fuel use by noncommercial passenger highway vehicles attributable to obesity.
Annual excess jet fuel use attributable to obesity(Node #362134)
Welfare costs(Node #362129)
Intangible costs of obesity(Node #370536)
The intangible costs associated with pain and suffering from obesity and obesity-associated conditions.
Mitigation costs(Node #367012)
Cost implications of deeming obesity to be a disability?(Node #370904)The European Court of Justice ruled in December 2014 that if obesity could hinder "full and effective participation" at work then it could count as a disability – and be covered by the protection provided for in EU Council Directive 2000/78/EC of 27 November 2000, which establishes a general framework for equal treatment in employment and occupation, and offers protection by the prohibition of discrimination on grounds of that disability.
Clive Coleman, BBC's legal correspondent
"Today's ruling was of great interest to employers across Europe. The judgement makes no direct link between Body Mass Index and obesity, but is a powerful statement that an obese worker whose weight hinders their performance at work is entitled to disability protection.
That will mean employers must, on a case by case basis, make reasonable adjustments such as providing larger chairs or special car parking, and protect such employees from verbal harassment.
But there are wider implications. Providers of goods and services such as shops, cinemas and restaurants will also have to make reasonable adjustments for their customers, which might include things like special seating arrangements.
The key concept here is that adjustments must be "reasonable" - so it may be deemed reasonable for a Premier League football club to make two seats available for someone disabled through obesity, but not for a small, non-league club.
Obesity, particularly what is sometimes known as morbid or severe and complex obesity, can be a particularly sensitive subject.
Employers and service providers will have to take care not to make assumptions about the needs of an obese worker or customer."
How to estimate the costs?(Node #371756)
What methods can be used to estimate the financial costs of obesity?
Incidence-based estimations(Node #371766)
Incidence-based estimations follow individuals in a study population, record their healthcare expenses over time, and compare the expenses of obese individuals with those of their normal-weight counterparts.
Enables statistical adjustment for multiple causes of observed costs(Node #371768)
Difficulty of tracking costs across lifetime to identify total costs(Node #371770)
Prevalence-based estimations(Node #371759)
Identify the prevalence of diseases incurred by obese individuals, the proportion of these diseases attributable to obesity (population attributable risk, or PAR), and their associated costs (direct costs attributable to obesity = PAR x average medical expenditure among all cases).
Data is readily available(Node #371760)
Results offer a snapshot of the annual cost of obesity(Node #371761)
Risk of double counting costs(Node #371763)
The overlap between different medical conditions introduce the risk of double counting costs.
Risk of omitting emerging costs from new obesity-related diseases(Node #371765)
UK figures may substantially underestimate the cost of obesity(Node #362028)Per capita comparisons with the estimated costs of obesity in Australia and the US, for example, suggest that the current UK estimates may substantially underestimate the financial cost of obesity to the nation.
Per capita comparison with Australia's obesity cost estimates(Node #371549)
Per capita comparisons with the estimated costs of obesity in Australia suggest that the current UK estimates may substantially underestimate the financial cost of obesity to the nation.
Per capita comparisons with the US's obesity cost estimates(Node #371550)
Per capita comparisons with the estimated costs of obesity in the United States of America suggest that the current UK estimates may substantially underestimate the financial cost of obesity to the nation.
Modelling suggests the majority of UK population may be obese by 2050(Node #348775)
The prevalence of obesity in the UK more than doubled in the 25 years to 2007. In England, nearly a quarter of adults and about 10% of children were obese in 2007, with a further 20–25% of children overweight. The Foresight report extrapolated that 40% of Britons might be being obese by 2025, with Britain being a mainly obese society by 2050.
Financial cost of obesity grows as the prevalence of obesity rises(Node #371552)
The cost of treating the health consequences of obesity, and productivity losses due to obesity, increase as the prevalence of obesity spreads in the population.
1 in 4 UK adults are obese(Node #366906)24.7 per cent of British adults are obese (compared with an average of 16.7 per cent in the rest of Europe) [1], [2] – and one out of four men (24.7%) and one of four women (24.9%) is obese in England. [4], [5]
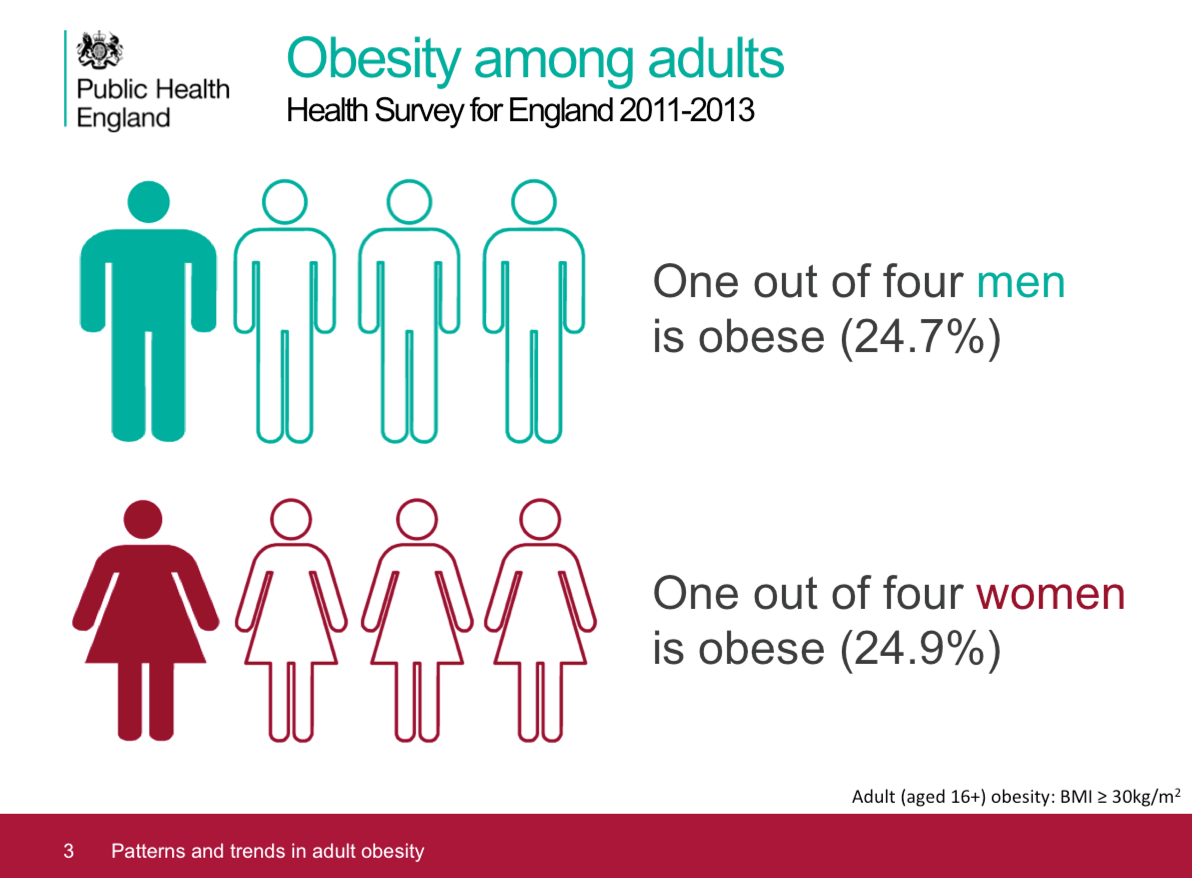
Source: PHE Adult obesity slide set (updated March 2015) [4] 1 in 5 UK children aged 10-11 are obese(Node #352358)The National Child Measurement Programme (NCMP) figures for 2013/14, show that 19.1% of children in Year 6 (aged 10-11) were obese and a further 14.4% were overweight. Obese children and adolescents are at an increased risk of developing various health problems—such as asthma, cardiovascular disease and type 2 diabetes (as well as low self-esteem and depression)—and are also more likely to become obese adults.
- The National Child Measurement Programme (NCMP) measures the height and weight of around one million school children in England every year, providing a detailed picture of the prevalence of child obesity.
- In addition to showing that 19.1% of children in Year 6 (aged 10-11) were obese and a further 14.4% were overweight, the figures for 2013/14 show that 9.5% of children in Reception (aged 4-5), were obese and another 13.1% were overweight (meaning that a third of 10-11 year olds and over a fifth of 4-5 year olds were overweight or obese. [1], [2]
- Results from the 2012 Health Survey for England (HSE)—which includes a smaller sample of children than the NCMP but covers a wider age range—show that around 28% of children aged 2 to 15 were classed as either overweight or obese. [1]
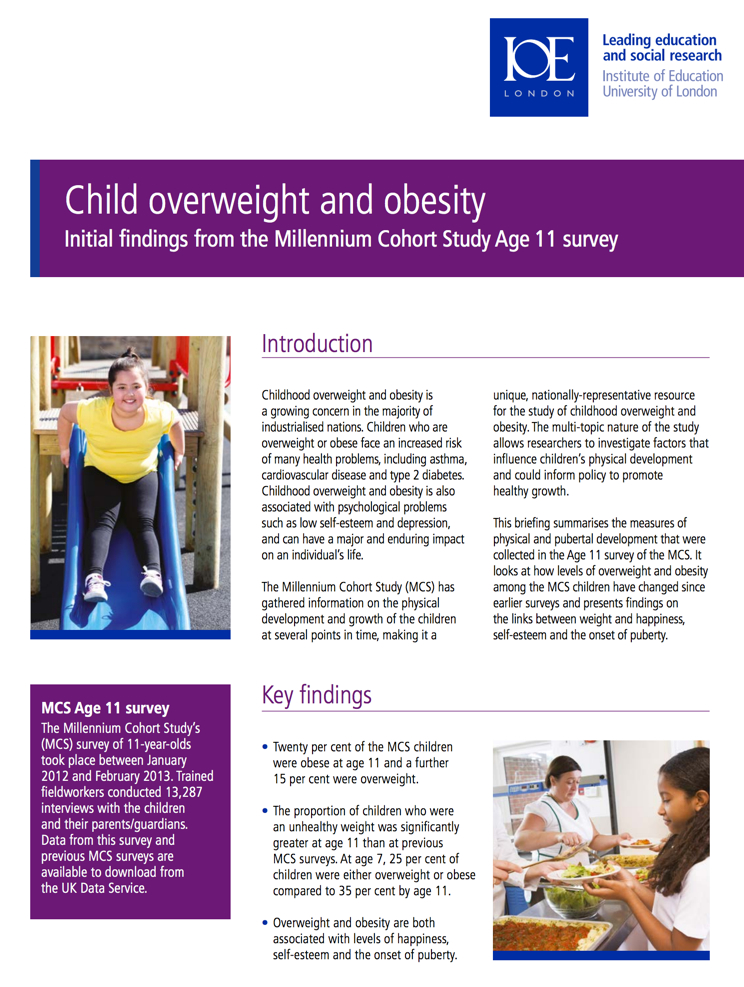
Link between divorce and childhood obesity(Node #362502)
A recent Norwegian study found that general and abdominal obesities were more prevalent among children of divorced parents.
Obesity harms children and young people(Node #374621) Emotional and behavioural impact on children(Node #374622)
Bullying(Node #374623)
Low self-esteem(Node #374625)
Stigmatisation of children(Node #374624)
Obesity's impacts on the health of children and young people(Node #374627)
Bone and Joint Problems(Node #374631)
Breathing difficulties(Node #374632)
High blood pressure(Node #374629)
High cholesterol(Node #374628)
Increased risk of adult ill-health and premature mortality(Node #374633)
Increased risk of becoming overweight adults, and of ill health and premature mortality in adult life.
Pre-diabetes(Node #374630)
School absence(Node #374626)
Two phases of childhood obesity(Node #390259)
Research reported in the International Journal of Obesity, which compares the obesity data in the 1980s with 307 present-day children, suggests that there may be two distinct phases of childhood obesity; one operating selectively according to parental BMI during early childhood, the second more generally in puberty and influenced more by peer-group factors. The finding suggests that different approaches may be needed to tackle the different phases of the problem.
UK's obesity rate ranks 132 out of 161 countries(Node #387193)The UK's obesity rate places it 132 out of 161 countries in the Social Progress Index 2015 – based on WHO data of the percentage of the population with a body mass index (BMI) of 30 kg/m2 or higher (age-standardized estimate), both sexes.
| Rank | Country | Obesity rate |
| 1 | Bangladesh | 1.1 |
| 2 | Ethiopia | 1.2 |
| 3 | Nepal | 1.5 |
| 4 | Vietnam | 1.6 |
| 5 | Madagascar | 1.7 |
| 6 | India | 1.9 |
| 7 | Congo, Democratic Republic of | 1.9 |
| 8 | Cambodia | 2.3 |
| 9 | Afghanistan | 2.4 |
| 10 | Burkina Faso | 2.4 |
| 11 | Niger | 2.5 |
| 12 | Timor-Leste | 2.9 |
| 13 | Laos | 3 |
| 14 | Chad | 3.1 |
| 15 | Burundi | 3.3 |
| 16 | Central African Republic | 3.7 |
| 17 | Myanmar | 4.1 |
| 18 | Zambia | 4.2 |
| 19 | Rwanda | 4.3 |
| 20 | Comoros | 4.4 |
| 21 | Japan | 4.5 |
| 22 | Malawi | 4.5 |
| 23 | Togo | 4.6 |
| 24 | Uganda | 4.6 |
| 25 | Guinea | 4.7 |
| 26 | Indonesia | 4.7 |
| 27 | Kenya | 4.7 |
| 28 | Mali | 4.8 |
| 29 | Sri Lanka | 5 |
| 30 | Congo, Republic of | 5.3 |
| 31 | Mozambique | 5.4 |
| 32 | Tanzania | 5.4 |
| 33 | Guinea-Bissau | 5.4 |
| 34 | Liberia | 5.5 |
| 35 | Bhutan | 5.5 |
| 36 | China | 5.6 |
| 37 | Pakistan | 5.9 |
| 38 | Philippines | 6.4 |
| 39 | Singapore | 6.4 |
| 40 | Benin | 6.5 |
| 41 | Sudan | 6.6 |
| 42 | Côte d'Ivoire | 6.7 |
| 43 | Sierra Leone | 7 |
| 44 | Nigeria | 7.1 |
| 45 | Angola | 7.2 |
| 46 | Korea, Republic of | 7.3 |
| 47 | Ghana | 8 |
| 48 | Senegal | 8 |
| 49 | Haiti | 8.4 |
| 50 | Thailand | 8.5 |
| 51 | Gambia, The | 8.5 |
| 52 | Zimbabwe | 8.6 |
| 53 | Tajikistan | 9.9 |
| 54 | Djibouti | 10.4 |
| 55 | Namibia | 10.9 |
| 56 | Cameroon | 11.1 |
| 57 | Cape Verde | 11.5 |
| 58 | Botswana | 13.5 |
| 59 | Mauritania | 14 |
| 60 | Malaysia | 14.1 |
| 61 | Turkmenistan | 14.3 |
| 62 | Switzerland | 14.9 |
| 63 | Gabon | 15 |
| 64 | France | 15.6 |
| 65 | Papua New Guinea | 15.9 |
| 66 | Denmark | 16.2 |
| 67 | Netherlands | 16.2 |
| 68 | Mongolia | 16.4 |
| 69 | Peru | 16.5 |
| 70 | Sweden | 16.6 |
| 71 | Yemen | 16.7 |
| 72 | Guyana | 16.9 |
| 73 | Lesotho | 16.9 |
| 74 | Italy | 17.2 |
| 75 | Kyrgyzstan | 17.2 |
| 76 | Morocco | 17.3 |
| 77 | Uzbekistan | 17.3 |
| 78 | Algeria | 17.5 |
| 79 | Greece | 17.5 |
| 80 | Romania | 17.7 |
| 81 | Colombia | 18.1 |
| 82 | Mauritius | 18.2 |
| 83 | Austria | 18.3 |
| 84 | Bolivia | 18.9 |
| 85 | Estonia | 18.9 |
| 86 | Belgium | 19.1 |
| 87 | Paraguay | 19.2 |
| 88 | Brazil | 19.5 |
| 89 | Honduras | 19.8 |
| 90 | Norway | 19.8 |
| 91 | Finland | 19.9 |
| 92 | Ukraine | 20.1 |
| 93 | Macedonia | 20.3 |
| 94 | Moldova | 20.4 |
| 95 | Cuba | 20.5 |
| 96 | Guatemala | 20.7 |
| 97 | Albania | 21.1 |
| 98 | Georgia | 21.2 |
| 99 | Croatia | 21.3 |
| 100 | Germany | 21.3 |
| 101 | Bulgaria | 21.4 |
| 102 | Iran | 21.6 |
| 103 | Portugal | 21.6 |
| 104 | Montenegro | 21.8 |
| 105 | Dominican Republic | 21.9 |
| 106 | Iceland | 21.9 |
| 107 | Ecuador | 22 |
| 108 | Latvia | 22 |
| 109 | Oman | 22 |
| 110 | Serbia | 23 |
| 111 | Poland | 23.2 |
| 112 | Armenia | 23.4 |
| 113 | Belarus | 23.4 |
| 114 | Cyprus | 23.4 |
| 115 | Swaziland | 23.4 |
| 116 | Luxembourg | 23.4 |
| 117 | Uruguay | 23.6 |
| 118 | Tunisia | 23.8 |
| 119 | Spain | 24.1 |
| 120 | Bosnia and Herzegovina | 24.2 |
| 121 | Nicaragua | 24.2 |
| 122 | Canada | 24.3 |
| 123 | Kazakhstan | 24.4 |
| 124 | Ireland | 24.5 |
| 125 | Costa Rica | 24.6 |
| 126 | Jamaica | 24.6 |
| 127 | Slovakia | 24.6 |
| 128 | Azerbaijan | 24.7 |
| 129 | Lithuania | 24.7 |
| 130 | Hungary | 24.8 |
| 131 | Russia | 24.9 |
| 132 | United Kingdom | 24.9 |
| 133 | Australia | 25.1 |
| 134 | Israel | 25.5 |
| 135 | Panama | 25.8 |
| 136 | Suriname | 25.8 |
| 137 | Malta | 26.6 |
| 138 | El Salvador | 26.9 |
| 139 | New Zealand | 27 |
| 140 | Slovenia | 27 |
| 141 | Lebanon | 28.2 |
| 142 | Czech Republic | 28.7 |
| 143 | Chile | 29.1 |
| 144 | Turkey | 29.3 |
| 145 | Argentina | 29.4 |
| 146 | Iraq | 29.4 |
| 147 | Trinidad and Tobago | 30 |
| 148 | Venezuela | 30.8 |
| 149 | Libya | 30.8 |
| 150 | Syria | 31.6 |
| 151 | United States | 31.8 |
| 152 | Bahrain | 32.6 |
| 153 | Mexico | 32.8 |
| 154 | Qatar | 33.1 |
| 155 | South Africa | 33.5 |
| 156 | United Arab Emirates | 33.7 |
| 157 | Jordan | 34.3 |
| 158 | Egypt | 34.6 |
| 159 | Belize | 34.9 |
| 160 | Saudi Arabia | 35.2 |
| 161 | Kuwait | 42.8 |
Tackling obesity(Node #348770)Many policy interventions have been suggested to address the obesity crisis across multiple studies—and indeed many such measures have been implemented, and are being implemented, now. There's recognition too that these interventions need to be part of a coherent and comprehensive whole systems strategy [4]; with some grounds for optimism that such an approach has the potential to accomplish a significant reduction in the prevalence of obesity in the UK across the next decade. [2]
Adopt a whole systems approach to obesity(Node #348675)Tackling obesity effectively—accomplishing a population wide-shift—requires a comprehensive and integrated whole systems approach, involving a range of measures focusing on individuals, social and other systems, including at the local and community level, and on the interrelated physical, physiological, social and cognitive factors that determine health outcomes.
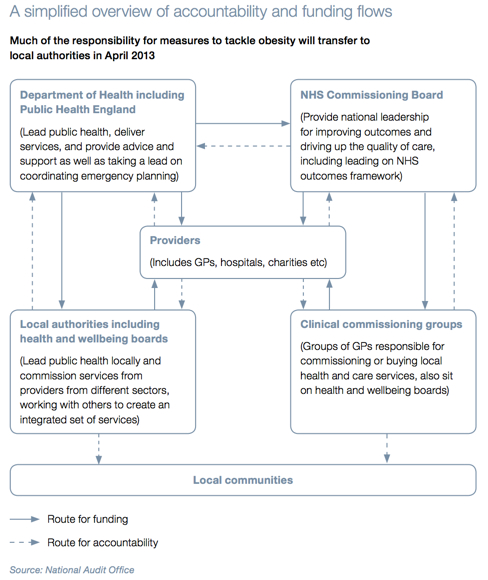
Deploy and integrate as many interventions as possible at scale(Node #366449)Commission and deploy as many interventions as possible at scale and delivered effectively, and integrated way, by the full range of sectors in society.

Source: MGI Overcoming Obesity
The main findings of the McKinsey Global Institute discussion paper include:
- Existing evidence indicates that no single intervention is likely to have a significant overall impact. A systemic, sustained portfolio of initiatives, delivered at scale, is needed to reverse the health burden. Almost all the identified interventions (exhibit) are cost effective for society—savings on healthcare costs and higher productivity could outweigh the direct investment required by the intervention when assessed over the full lifetime of the target population. In the United Kingdom, for instance, such a program could reverse rising obesity, saving the National Health Service about $1.2 billion a year.
Cost-effective interventions to reduce obesity in the UK
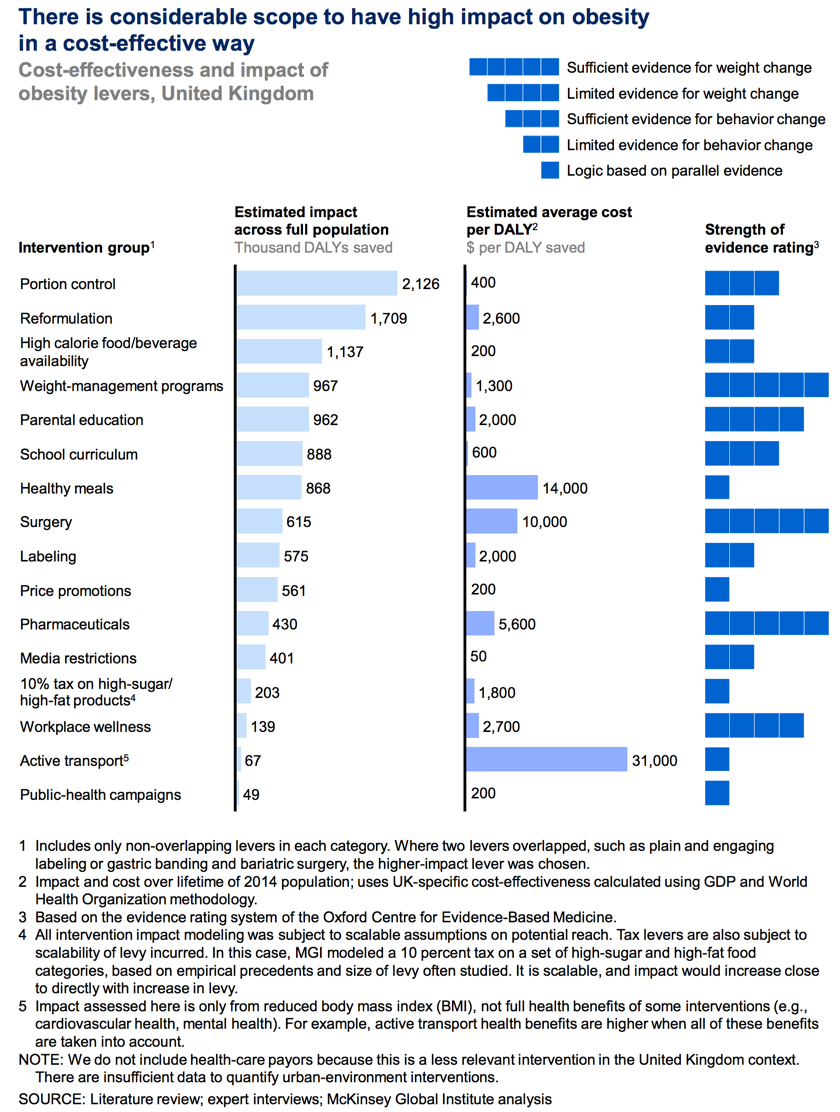
- Education and personal responsibility are critical elements of any program aiming to reduce obesity, but they are not sufficient on their own. Other required interventions rely less on conscious choices by individuals and more on changes to the environment and societal norms. They include reducing default portion sizes, changing marketing practices, and restructuring urban and education environments to facilitate physical activities.
- No individual sector in society can address obesity on its own—not governments, retailers, consumer-goods companies, restaurants, employers, media organizations, educators, healthcare providers, or individuals. Capturing the full potential impact requires engagement from as many sectors as possible. Successful precedents suggest that a combination of top-down corporate and government interventions, together with bottom-up community-led ones, will be required to change public-health outcomes. Moreover, some kind of coordination will probably be required to capture potentially high-impact industry interventions, since any first mover faces market-share risks.
- Implementing an obesity-abatement program on the required scale will not be easy. We see four imperatives:
(1) as many interventions as possible should be deployed at scale and delivered effectively by the full range of sectors in society;
(2) understanding how to align incentives and build cooperation will be critical to success;
(3) there should not be an undue focus on prioritizing interventions, as this can hamper constructive action; and
(4) while investment in research should continue, society should also engage in trial and error, particularly where risks are low.
Experiment with multiple interventions(Node #366462)
Society should be prepared to experiment with possible interventions. In many intervention areas, impact data from high-quality, randomized control trials are not possible to gather. So, rather than waiting for such data, the relevant sectors of society should be pragmatic with a bias toward action, especially where the risks of intervening are low, using trial and error to flesh out their understanding of potential solutions.
Education and personal responsibility are necessary but not sufficient(Node #366454)
Education and encouraging personal responsibility are necessary but not sufficient.
Many interventions are highly cost-effective(Node #366453)
Almost all of the interventions we analyzed are highly cost-effective from the viewpoint of society.
Need to reshape the physical activity and nutritional environment(Node #366455)
Restructuring the context that shapes physical activity and nutritional behavior is a vital part of any obesity program.
No single solution creates sufficient impact to reverse obesity(Node #366452)
No single solution creates sufficient impact to reverse obesity: only a comprehensive, systemic program of multiple interventions is likely to be effective.
Improve collaboration across organisational boundaries(Node #372559)Effective collaboration across organisational boundaries is vital to achieving and sustaining constructive progress in the face of complex, systemic problems—and to leveraging the energy, insight and resources distributed across the network of organisations to maximum effect.
Appoint an obesity champion or tsar(Node #362143)
Appoint a government obesity champion to drive a coordinated obesity strategy between and across central government departments which include Health, the Treasury, Sport, Education, Agriculture, the Department of Work and Pensions, and local government for the local environment. This person should have a strong but politically independent status (e.g. a member of the House of Lords) with the skills and authority to address issues which need multiple government departmental involvement.
Every local authority should have an obesity champion(Node #352564)
Ability to work across institutional boundaries(Node #371396)
"Tsar" label has proved counterproductive in the past(Node #372561)
Previous Tsars, across various policy areas, have observed that they found the "tsar" label to be counterproductive to their work.
Interconnecting across existing hierarchies may be more effective(Node #373443)
Analysis of the US intelligence community, using small-world network metrics of Watts & Strogatz [2], suggests that a strategy of interconnecting effectively across hierarchies – allied to the associated changes organisational culture that demand and reward knowledge sharing – may be more effective than introducing a Tsar.[1]
Create a whole-systems, cross-sector learning collaborative on obesity(Node #371076)
Key questions for a whole systems approach(Node #351678)
A set of key questions for a whole systems approach identified by the National Institute for Health and Care Excellence.
1. Key elements of a whole-system approach?(Node #351679)
What are the essential elements of a robust, community-based, whole-system approach to preventing obesity (for example, societal, environmental and organisational)?
How do they interact with each other?(Node #351680)
How do the essential elements of a robust, community-based, whole-system approach to preventing obesity interact with each other?
2. How do local and national policy interact?(Node #351683)How does local and national policy impact on the effectiveness, cost effectiveness, delivery and sustainability of local action to prevent obesity? Are there any unintentional consequences?
- For example, policies on health and transport may conflict, if people are being encouraged to be physically active but are living in environments dominated by busy roads.
3. What packages of action are effective?(Node #351685)
What ‘packages’ of actions and strategies may be effective and cost effective in bringing about population-wide improvements in weight management within a given community? How does effectiveness vary between different communities or population groups, including disadvantaged groups?
How does effectiveness vary between different communities?(Node #351687)
How does effectiveness vary between different communities or population groups, including disadvantaged groups?
What packages of action are cost-effective?(Node #351686)
What ‘packages’ of actions and strategies may be effective and cost effective in bringing about population-wide improvements in weight management within a given community?
4. Barriers and facilitators?(Node #351688)
What barriers and facilitators may influence the implementation, delivery and effectiveness of these ‘packages’ of actions and strategies among a given community? (This should include any barriers and facilitators for specific groups)
Barriers to effectiveness?(Node #351689)
What barriers may impede the implementation, delivery and effectiveness of these ‘packages’ of actions and strategies among a given community?
Facilitators of effectiveness?(Node #351690)
What facilitators may enhance the implementation, delivery and effectiveness of these ‘packages’ of actions and strategies among a given community?
5. Essential partners?(Node #351691)
Who are the essential partners (formal and informal)?
6. How can multiple factors be tackled simultaneously?(Node #351692)
How can local political, social, economic and environmental factors be tackled simultaneously as part of a whole-system approach to preventing obesity?
Encourage transdisciplinary research(Node #352937)
Charles Perkins Centre(Node #352938)The Charles Perkins Centre aims to ease the burden of obesity, diabetes and cardiovascular disease by translating the work of the University of Sydney into real-world solutions. At the heart of the Charles Perkins Centre is a $385 million research and education hub.
Set up a COBRA-style emergency taskforce on childhood obesity(Node #372560)
Set up a COBRA-style emergency taskforce—a national Child Obesity Action Group (COAG)—to tackle the rising epidemic of childhood obesity.
Involve all stakeholders in the process of change(Node #348779)
Reversing the rising trend and addressing the prospect of the rising health burden and societal costs will be demanding and will necessitate major changes in behaviour – not only in individuals, but also in families, communities, organisations and economic markets.
Understand how to align incentives and build cooperation(Node #366450)
Bring together coalitions of local partners(Node #352810)
Co-ordinated multi-party actions are required to tackle obesity(Node #366456)
Capturing the full potential impact is likely to require commitment from government, employers, educators, retailers, restaurants, and food and beverage manufacturers, and a combination of top-down corporate and government interventions and bottom-up community-based ones.
Target interventions across the whole course of life(Node #352312)
Tackling obesity effectively requires the adoption of a life course approach – from pre-conception through pregnancy, infancy, early years, childhood, adolescence and teenage years, and through to adulthood and preparing for older age. There are specific opportunities and challenges at each stage of the life course and action is needed at all ages to avert the short- and long-term consequences of excess weight and to ensure that health inequalities are addressed.
Set clear, long-term societal goals and deepen the sense of urgency(Node #352786)
Establish both a clear aim-statement for long-term, systemic change and the sense of urgency to achieve this systemic change.
Changes required across many different policy areas(Node #352281)Obesity has to be seen as not just a technical, food, physical activity or healthcare problem but a challenge for what sort of society is being built. Small, incremental, publicity-driven (i.e. social market-based) changes might suit the existing balance of policy interests, but a more extensive, co-ordinated, cross-sectoral action would be more effective.
Encouraging daily physical activity and modifying dietary intake raises complex questions for public policy across a number of areas; including:
- agriculture – because policy affects what is produced;
- manufacturing – for ingredients, portions and products;
- retail – for planning, prices, availability and location;
- education – for health knowledge and skills;
- culture – for the shaping of consciousness around food and physical activity;
- trade – for product pricing and terms of trade;
- economics – for differential taxation and subsidy of foods.
Causal factors in one domain thwart progress in other domains(Node #366808)
Current policies are failing because they do not cover the range and depth of interventions needed. New policy on obesity has to cover the entire terrain, or continued drivers in one dimension might undermine positive action in others. There may be little payoff from working on one aspect of obesity without tackling other determinants as well.
Who should adopt a whole systems approach to obesity?(Node #400394)
Improve obesity training for healthcare professionals(Node #396117)Improve systems of obesity education and training across all health professional groups to ensure that all professional primary and secondary healthcare groups are appropriately competent to respond to the demands of the obesity crisis.
From the NICE Guidelines: [8]
"Those responsible for setting competences and continuing professional development programmes for health professionals (including local education and training boards; local education and training councils and professional bodies) should:
- Ensure professional development training on weight management is available for health and social care professionals.
- Train GPs and other health and social care professionals to identify when to raise weight management with someone and to do so confidently, but with empathy. They should understand why many adults have difficulty managing their weight and the experiences they may face in relation to it. This includes considering the effect of their attitudes to, and any concerns about, their own weight.
- Train GPs and other health and social care professionals to accurately measure and record height and weight, determine BMI and accurately measure waist circumference.
- Train GPs and other health and social care professionals to understand the practical skills and behaviours that can help someone lose or maintain their weight and how to provide ongoing support and encouragement. This includes encouraging people to self-manage and self-monitor their weight and any associated behaviours over the long term.
- Train GPs and other health and social care professionals to discuss the likely benefits of a lifestyle weight management programme with service users, taking into account someone's personal circumstances. For example, they should take into account any associated medical conditions or personal factors, such as someone's commitment to change.
- Train GPs and other health and social care professionals in how to help people make an informed decision about the best weight management option for them. They should also be able to refer people to the most appropriate weight management service. This includes identifying people with more complex needs and referring them to appropriate services (such as mental health, psychological or alcohol services).
- Train GPs and other health and social care professionals to identify when someone may benefit from re-referral to a lifestyle weight management programme."
Characteristics of good obesity training?(Node #396116)Characteristics of good obesity training for healthcare professionals?
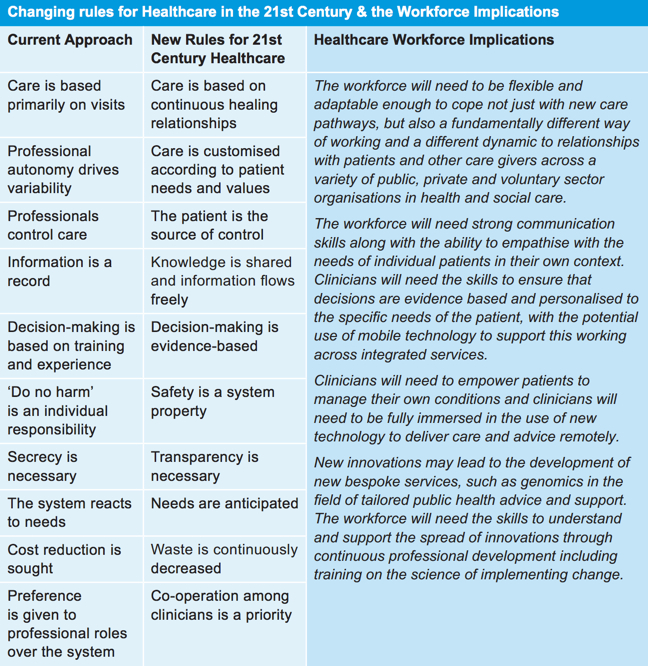
Source: HEE [1] via IOM [2] and Kings Fund [3]
Training should reflect the different needs of different team members(Node #370342)
Different members of the team will need different training. For example, the role of the GP in an initial consultation differs greatly from that of the bariatric surgeon and his or her team assessing a patient’s suitability for surgery. Different teams need different skills for different patients in different scenarios but healthcare professionals’ education.
Require and examine obesity knowledge as part of curricula(Node #370336)
Knowledge, understanding and training in nutrition, physical activity, exercise and the public health aspects of obesity should be an essential part of undergraduate and postgraduate curricula in every discipline because complications of obesity cross all specialty and professional boundaries. This knowledge should be examined.
Training should include sensitive recognition and appropriate referral(Node #370346)
All health professionals should have some basic training in sensitive recognition and appropriate referral for overweight and obese patients.
Improved GP training on obesity(Node #348684)GPs should be provided with appropriate support and training to help them have the necessary conversations with patients. Better quality training should be provided both during GP training and for current GPs to help them provide better advice to patients. [1]
- The Department of Health should encourage training and accreditation schemes that exist on this subject, as these will help GPs in making every contact with patients count.
- The training includes increasing awareness amongst GPs of the importance of waist measurement during medical appointments in order to identify indicators of visceral adiposity or ectopic fat deposits, which can adversely affect health outcomes.
GPs should have appropriate training to provide useful advice to patients.
Need to make every contact with patients count(Node #348680)GPs and other health professionals should be encouraged and required to make every contact with patients count. Very few patients will cite obesity or weight management as the reason for seeing their GP, and will instead present with conditions that are clearly a result of weight issues. GPs should talk with their patients about weight in these instances. [1]
GPs should measure waist circumference(Node #348704)
GPs should measure waist circumference rather than just BMI to help them identify patients who are most at risk and identify the indicators of poor health outcomes. [1]
Understand the ten essential facts about obesity(Node #370327)All healthcare professionals should know and understand the ‘Ten essential facts about obesity’.
The Royal College of Physicians [1] notes that:
- In the UK 1 in 4 adults are obese (2012).
- In the UK 1 in 5 children aged 10–11 are obese (2011).
- Obesity is strongly heritable (60% of weight variance is attributed to heredity) yet currently known gene mutations and polymorphisms account for <5% of weight variability.
- Diagnosis by BMI requires measuring height and weight accurately; risk stratification in overweight and modest obesity requires measuring waist circumference and possibly the use of a clinical staging system (Edmonton Obesity Staging System (EOSS)).
- Prevention and long-term weight loss maintenance require sustained changes in diet and physical activity habits.
- Obesity is a major risk factor in diabetes (5 x), cancer (3 x the risk of colon cancer), and heart disease (2.5 x).
- Obesity is a major cause of health inequality and impaired quality of life and costs the NHS £5.0bn per year (2012).
- Modest weight loss (~10 kg) helps to improve diabetes, improves quality of life and reduces morbidity.
- An energy deficit of only 100 calories per day predicts a 0.5 kg weight loss in a month.
- Cost-effective treatments in appropriate patients include weight loss programmes (commercial: e.g. WeightWatchers; GP delivered: eg Counterweight); pharmacotherapy (egorlistat); and bariatric surgery.
Existing training is inadequate and ineffective(Node #352560)
Traditional methods of training for healthcare professionals are inadequate and ineffective with respect to obesity.
GPs rarely use interventions for weight management(Node #372996)Research published in the BMJ in 2015 suggests that few UK family doctors seem to be treating overweight and obese patients appropriately, with some not treating it all – and that, where interventions are used, follow up to determine their success is poor.
From the BMJ Press Release: [2]
"Few UK family doctors seem to be treating overweight/obesity appropriately, with some not treating it all, suggests an analysis of patient records published in the online journal BMJ Open.
The researchers scrutinised the anonymised health records of more than 90,000 obese and overweight adults, whose data had been entered into the Clinical Practice Research Datalink (CPRD) between 2005 and 2012.
The CPRD is the largest primary care database in the world, and contains the health records of over 5% of the UK population, submitted by 680 general practices.
The researchers looked at all the weight management options provided, including lifestyle advice, specialist referrals, and prescription of obesity drugs.
The average age of the patients was 56. Some 60% were overweight and 40% were obese, including 5% who were morbidly obese with a body mass index (BMI) of 40kg/m2 or more.
Between 2005 and 2012, no weight management intervention was recorded for most (90%) of the overweight patients. Many practices didn't record any interventions at all for obese patients during this time.
A weight management intervention was more likely to be recorded in the health records of obese patients, but it was still not documented in more than 80% of those with simple obesity.
Patients with severe obesity were more than three times as likely to be offered weight management, but this was still not recorded in the case notes of over half (59%) of them.
Lifestyle change, including dietary advice and exercise, was the most common weight management plan offered in all but the most severely obese patients, for whom drug treatment was the most commonly recorded intervention.
And there was little documented evidence that progress on weight loss had been tracked after an intervention had been introduced.
Monitoring progress on weight loss in the first year after an intervention was most frequently recorded in the case notes of patients who had been referred to specialist services (34%). But it was only recorded for one in five of those given lifestyle advice and one in four of those prescribed an obesity drug.
There was no evidence that outcomes were being monitored for any intervention after five years.
Factors associated with weight loss intervention included older age, type 2 diabetes, and depression, with morbid obesity the strongest predictor of weight management provision. Women, former smokers, and those from disadvantaged backgrounds were also more likely to be treated for overweight/obesity.
The researchers point out that the findings might simply be the result of poor documentation, and that brief advice may have been offered, but not recorded in the patient's notes.
On the other hand, the findings "might also indicate a lack of patient access to appropriate body weight management interventions in primary care due to a lack of clinician awareness or confidence in treating obesity," they write.
The reasons for this might include too little time to tackle the issue in consultations, doubts about the success of weight loss attempts, greater use of drugs to treat obesity related risk factors and disease, and possibly 'normalisation' of excessive body weight.
Nevertheless, they conclude:
"The results of this study suggest that primary care interventions given to patients with the aim of reducing weight are underutilised, and that follow up to determine their success is poor."
And they emphasise:
"The growing burden of obesity on primary healthcare services and lack of long term follow up on the effectiveness of these treatments supports the use of structured recording of interventions for weight management."
Many health professionals still have inadequate knowledge(Node #370326)Many recently trained health professionals still have an inadequate knowledge of the nutritional aspects of health promotion and disease treatment and the potential benefits of regular physical activity.
In a 2010 review of the training of health professionals for prevention and treatment of overweight and obesity, the Royal College of Physicians concluded [4] that:
‘health professionals either lack appreciation of the health and medical consequences of obesity or lack confidence and the ability to help […and…] too often health professionals ignore the obvious signs or symptoms of obesity or simply instruct the individual to go on a diet and lose significant weight.’
Similarly, Professor Anthony Leeds of the University of Surrey has highlighted [3] the fact that specific training on obesity management is missing from most GP training programmes, and most GPs are better equipped to deal with the consequences of obesity, such as heart disease, type-2 diabetes, and osteoarthritis, than they are to help patients deal with the underlying weight gain which has caused the problem.
Tags: Doctor, Doctors, Nurse, Nurses Knowledge gaps on obesity guidelines(Node #381550)
A US study [1] designed to assess the knowledge and practice patterns of primary care physicians (PCPs), endocrinologists (ENDOs), cardiologists (CARDs) and bariatricians (BARIs) regarding obesity found that respondents demonstrated knowledge gaps on obesity guidelines.
Knowledge gaps on pathophysiology (Node #381551)
A US study [1] designed to assess the knowledge and practice patterns of primary care physicians (PCPs), endocrinologists (ENDOs), cardiologists (CARDs) and bariatricians (BARIs) regarding obesity found that respondents demonstrated knowledge gaps on pathophysiology.
Lack of understanding of obesity medication efficacy and safety(Node #381552)
A US study [1] designed to assess the knowledge and practice patterns of primary care physicians (PCPs), endocrinologists (ENDOs), cardiologists (CARDs) and bariatricians (BARIs) regarding obesity found that respondents generally lacked understanding of obesity medication efficacy, safety and MOA.
Obesity and nutrition are underrepresented in medical curriculum(Node #352568)
Education in obesity and nutrition are inadequately represented in the current medical undergraduate curriculum.
Some clinicians are insensitive in dealing with obese patients(Node #370328)
Some clinicians continue to be insensitive, ineffective, and lack confidence when dealing with patients who have problems with their weight.
Many healthcare professionals are overweight and obese(Node #370335)
Doctors continue to be a trusted and respected source of advice and guidance for patients over their lifestyle choices; however, many healthcare professional struggle with their own weight which can make them less effective both as messengers and exemplars.
NHS Five Year Forward View depends on improved training(Node #373004)
Without additional training of GPs and other frontline healthcare professionals, and increased availability of weight management services, the plans set out for the Five Year Forward View will be undermined.
Who should improve obesity training for healthcare professionals?(Node #352713)
Who should improve systems of obesity education and training across all health professional groups to ensure that all professional primary and secondary healthcare groups are appropriately competent to respond to the demands of the obesity crisis.
Improve public education, literacy & actions on obesity and nutrition(Node #400390)
Improve public education, literacy and actions on obesity and nutrition and health. Ensure that all citizens have a requisite level of food choosing, sourcing and preparation, and general food literacy.
Encourage individuals and families to make healthier choices(Node #366559)
A healthier diet(Node #348691)
Encourage people to eat a healthier diet – and to be more health-discerning about when, how often, and what to eat.
Better balance between energy intake and energy expenditure(Node #348764)
The Eat Well Plate(Node #370211)The eatwell plate highlights the different types of food that make up our diet, and shows the proportions we should eat them in to have a well balanced and healthy diet.
It's a good idea to try to get this balance right every day, but you don't need to do it at every meal. And you might find it easier to get the balance right over a longer period, say a week. Try to choose options that are lower in salt when you can.
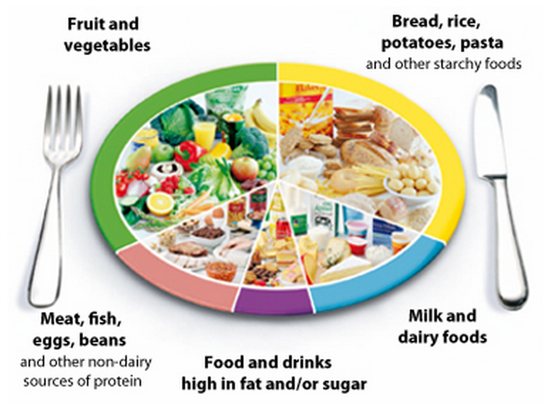
Eating healthily is about eating the right amount of food for your energy needs. In England, most adults are either overweight or obese. This means many of us are eating more than we need, and should eat and drink fewer calories in order to lose weight.
Based on the eatwell plate, try to eat:
- Plenty of fruit and vegetables: Did you know that we should be eating at least five portions of a variety of fruit and veg every day?
- Plenty of potatoes, bread, rice, pasta and other starchy foods: Choose wholegrain varieties whenever you can, or eat potatoes with their skins on for more fibre.
- Some milk and dairy foods: Go for lower-fat milk and dairy foods. These are healthier options to help you get enough protein and calcium.
- Some meat, fish, eggs, beans and other non-dairy sources of protein: These are important sources of protein, vitamins and minerals, and form part of a healthy balanced diet.
- Just a small amount of foods and drinks that are high in fat or sugar: Cut down on fat and sugar by eating fewer sweets, cakes and biscuits, and drinking fewer sugary soft drinks.
Is the eatwell plate for me?
The eatwell plate applies to most people – whether they're a healthy weight or overweight, whether they eat meat or are vegetarian, and no matter what their ethnic origin.
However, it doesn't apply to children under the age of two because they have different nutritional needs. Between the ages of two and five, children should gradually move to eating the same foods as the rest of the family, in the proportions shown on the eatwell plate.
Anyone with special dietary requirements or medical needs might want to check with a registered dietitian whether the eatwell plate applies to them.
Eatwell plate comparison for low income and all households(Node #371567)Household food purchases do not generally match the Government recommended Eatwell plate proportions of the types of food which make up a well balanced diet. Both low income households and all households have a relatively similar diet in terms of the Eatwell Plate categories.
WHO – Healthy Diet(Node #371154)The World Health Organization's fact sheet on healthy diet.

Key facts
- A healthy diet helps protect against malnutrition in all its forms, as well as noncommunicable diseases (NCDs), including obesity, diabetes, heart disease, stroke and cancer.
- Unhealthy diet and lack of physical activity are leading global risks to health.
- Healthy dietary practices start early in life – breastfeeding may have longer-term benefits, like reducing the risk of overweight and obesity in childhood and adolescence.
- Energy intake (calories) should balance energy expenditure. Evidence indicates that total fat should not exceed 30% of total energy intake to avoid unhealthy weight gain [2] , [3], [4], with a shift in fat consumption away from saturated fats to unsaturated fats [4], and towards the elimination of industrial trans fats [5].
- Limiting intake of free sugars to less than 10% of total energy [3], [6] is part of a healthy diet. A further reduction to less than 5% of total energy [7] is suggested for additional health benefits.
- Keeping salt intake to less than 5 g per day helps prevent hypertension and reduces the risk of heart disease and stroke in adult population. [8]
- WHO Member States have agreed to reduce the global population’s intake of salt by 30% and halt the rise in diabetes and obesity by 2025.
Overview
Consuming a healthy diet throughout the life-course helps prevent malnutrition in all its forms as well as a range of noncommunicable diseases (NCDs) and conditions. But increasing production of processed food, rapid urbanization and changing lifestyles have led to a shift in dietary patterns. People are consuming more foods high in energy, saturated fats, trans fats, free sugars or salt/sodium, and many do not eat enough fruit, vegetables and dietary fibre such as whole grains.
The exact make-up of a healthy, balanced diet will vary depending on the individual needs (e.g. age, gender, lifestyle, degree of physical activity).
For adults
A healthy diet contains:
- fruits, vegetables, legumes (e.g. lentils, beans), nuts and whole grains (e.g. unprocessed maize, millet, oats, wheat, brown rice);
- at least 400 g (5 portions) of fruit and vegetables a day [3]. Potatoes, sweet potatoes, cassava and other starchy roots are not classified as fruits or vegetables;
- less than 10% of total energy from free sugars [3], [6] equivalent to 50g (or around 12 level teaspoons), but possibly less than 5% of total energy for additional health benefits. [7] Most free sugars are added to foods by the manufacturer, cook or consumer, and can also be found in sugars naturally present in honey, syrups, fruit juices and fruit concentrates;
- less than 30% of total energy from fat. [2], [3], [4] Unsaturated fats (e.g. found in fish, avocado, nuts, sunflower, canola and olive oils) are preferable to saturated fats (e.g. found in fatty meat, butter, palm and coconut oil, cream, cheese, ghee and lard). [4] Industrial trans fats (found in processed food, fast food, snack food, fried food, frozen pizza, pies, cookies, margarines and spreads) are not part of a healthy diet;
- less than 5 g of salt (equivalent to approximately one teaspoon) per day [8] and use iodized salt.
Infants and young children
The first 2 years of a child’s life are vital as optimal nutrition during this period reduces the risk of dying and of developing NCDs. It also fosters better development and healthy growth and development overall.
Advice on a healthy diet for infants and children is similar to that for adults but these elements are also important.
- Infants should be breastfed exclusively for the first 6 months of life.
- Infants should be continuously breastfed until 2 years and beyond.
- From 6 months of age, breast milk should be complemented with a variety of adequate, safe and nutrient dense complementary foods. Salt and sugars should not be added to complementary foods.
Practical advice on how to have a healthy diet
Fruit and vegetables
Eating at least 5 portions, or 400 g, of fruit and vegetables per day reduces the risk of NCDs [3], and helps ensure an adequate daily intake of dietary fibre.
In order to improve fruit and vegetable consumption you can:
- always include vegetables in your meals;
- eat fruit and raw vegetables as snacks;
- eat fresh vegetables in season;
- vary choices of fruits and vegetables.
Fats
Reducing the amount of total fat intake to less than 30% of total energy helps prevent unhealthy weight gain in adult population. [2], [3], [4]
Also, the risk of developing NCDs is lowered by reducing saturated fats to less than 10% of total energy, [3], [4] and trans fats to less than 1% of total energy, and replacing them with unsaturated fats contained in vegetable oils. [3], [4]
Fats intake can be reduced by:
- changing how you cook – remove the fatty part of meat; instead of butter, use vegetable oil (not animal); and boil, steam or bake rather than fry;
- avoid processed foods containing trans fats;
- limit the consumption of foods containing high amounts of saturated fats (e.g. cheese, ice creams, fatty meat).
Salt, sodium and potassium
Most people consume too much sodium through salt (corresponding to an average of 9–12 g of salt per day) and not enough potassium. High salt consumption and insufficient potassium intake (less than 3.5 g) contribute to high blood pressure, which in turn increases the risk of heart disease and stroke. [9]
Millions of deaths could be prevented each year if people’s salt consumption were reduced to the recommended level of less than 5 g per day.
People are often unaware of the amount of salt they consume. In many countries, most salt comes from processed foods (e.g. ready meals, processed meats like bacon, ham and salami, cheese and salty snacks) or from food consumed frequently in large amounts (e.g. bread). Salt is also added to food during cooking (e.g. bouillon, stock cubes) or at the table (e.g. table salt, soy sauce and fish sauce).
You can reduce salt consumption by:
- not adding salt, soy sauce or fish sauce during the preparation of food;
- not having salt on the table;
- limiting the consumption of salty snacks;
- choosing products with lower sodium content.
Some food manufacturers are reformulating recipes to reduce the salt content of their products, and it is good to check food labels to see how much sodium is in a product.
Potassium, which can mitigate the negative effects of elevated sodium consumption on blood pressure, can be increased with consumption of fruits and vegetables.
Sugars
Evidence indicates that intake of free sugars by adults and children should not exceed 10% of total energy [3], [6], and that a reduction of under 5% of total energy provides additional health benefits. [7] Free sugars are all sugars added to food or drinks by the manufacturer, cook or consumer, as well as sugars naturally present in honey, syrups, fruit juices and concentrates. [3]
Consuming free sugars increases the risk of dental caries (tooth decay). Excess calories from foods and drinks high in free sugars also contribute to unhealthy weight gain, which can lead to overweight and obesity.
Sugars intake can be reduced by:
- limiting the consumption of foods and drinks containing high amounts of sugars (i.e. sugar-sweetened beverages, sugary snacks and candies); eating fruit and raw vegetables as snacks instead of sugary snacks.
How to promote healthy diets
Diet can depend on an individual’s food choices, but also the availability and affordability of healthy foods, and sociocultural factors. Therefore, promoting a healthy food environment requires involvement across multiple sectors and stakeholders, including government, public and the private sector.
Governments have a central role in creating a healthy food environment that enables people to adopt and maintain healthy dietary practices.
Effective actions by policy-makers include:
- Coordinate trade, food and agricultural policies with the protection and promotion of public health:
- increase incentives for producers and retailers to grow, use and sell fruits and vegetables;
- reduce incentives for the food industry to use saturated fats and free sugars;
- set and enforce targets to reformulate food products to cut the contents of salt, fats (i.e. saturated fats and trans fats) and free sugars;
- implement the WHO recommendations on the marketing of foods and non-alcoholic beverages to children;
- establish standards to promote healthy, safe and affordable food in public institutions;
- encourage private companies to provide healthy food in their workplaces;
- set incentives and rules so consumers have healthy, safe and affordable food choices;
- encourage transnational, national and local food services and catering outlets to improve the nutritional quality of their food, create real choices, and review portion size and price;
- consider taxes and subsidies to encourage food manufacturers to produce healthier food and make healthy products available and affordable.
- Encourage consumers demand for healthy foods and meals:
- promote consumer awareness;
- develop school policies and programmes that encourage children to adopt a healthy diet;
- educate children, adolescents and adults about nutrition and healthy dietary practices;
- encourage culinary skills, including in schools;
- allow informed choices through proper food labelling that ensures accurate, standardized and comprehensible information on food content in line with the Codex Alimentarius Commission guidelines;
- provide dietary counselling in primary health care.
- Promote healthy nutrition in infants and young children:
- implement the International Code of Marketing of Breast-milk Substitutes
- promote and support breastfeeding in health services and the community, including through the Baby-Friendly Hospital Initiative.
5 A DAY(Node #371364)The 5 A DAY message highlights the health benefits of getting five 80g portions of fruit and vegetables every day. That's five portions of fruit and veg in total, not five portions of each.

5 A DAY is based on advice from the World Health Organization, which recommends eating a minimum of 400g of fruit and vegetables a day to lower the risk of serious health problems, such as heart disease,stroke, type 2 diabetes and obesity.
Five reasons to eat five portions of fruit and veg
- Fruit and vegetables are a good source of vitamins and minerals, including folate, vitamin C and potassium.
- They're an excellent source of dietary fibre, which helps maintain a healthy gut and prevent constipation and other digestion problems. A diet high in fibre can also reduce your risk of bowel cancer.
- They can help reduce the risk of heart disease, stroke and some cancers.
- Fruit and vegetables contribute to a healthy and balanced diet.
- Fruit and vegetables taste delicious and there's so much variety to choose from.
Fruit and vegetables are also usually low in fat and calories (provided you don't fry them or roast them in lots of oil). That's why eating them can help you maintain a healthy weight and keep your heart healthy.
To get the most benefit out of your 5 A DAY, your five portions should include a variety of fruit and vegetables. This is because different fruits and vegetables contain different combinations of fibre, vitamins, minerals and other nutrients.
Almost all fruit and vegetables count towards your 5 A DAY. They can be fresh, frozen, canned, dried or pure juices. Potatoes and cassava don't count because they mainly contribute starch to the diet.
To learn more about what counts towards your 5 A DAY, go to 5 A DAY: what counts?
WCRF & AICR Recommendations(Node #351185)
Recommendations from the World Cancer Research Fund and the American Institute for Cancer Research on food, nutrition, physical activity, and the prevention of cancer.
1. Be as lean as possible within the normal range of body weight(Node #351190)
Maintenance of a healthy weight throughout life may be one of the most important ways to protect against cancer. This will also protect against a number of other common chronic diseases.
2. Be physically active as part of everyday life(Node #351191)
Most populations, and people living in industrialised and urban settings, have habitual levels of activity below levels to which humans are adapted.
3. Limit consumption of energy-dense foods and avoid sugary drinks(Node #351192)
Consumption of energy-dense foods and sugary drinks is increasing worldwide and is probably contributing to the global increase in obesity.
4. Eat mostly foods of plant origin(Node #351193)
An integrated approach to the evidence shows that most diets that are protective against cancer are mainly made up from foods of plant origin.
Why is fibre important in obesity?(Node #351150)
1. Fibre reduces rate of intestinal carbohydrate absorption(Node #351151)
...which reduces insulin response.
2. Fibre induces satiety(Node #351152)
...by increasing speed of transit intestinal contents to ileum, to raise PYY 3-36, and induce satiety.
3. Fibre inhibits absorption of some free fatty acids to the colon(Node #351153)
...which are metabolized by colonic bacteria to short-chain fatty acids (SCFA) which suppress insulin.
5. Limit intake of red meat and avoid processed meat(Node #351194)
An integrated approach to the evidence also shows that many foods of animal origin are nourishing and healthy if consumed in modest amounts.
6. Limit alcoholic drinks(Node #351195)
The evidence on cancer justifies a recommendation not to drink alcoholic drinks. Other evidence shows that modest amounts of alcoholic drinks are likely to reduce the risk of coronary heart disease.
7. Limit consumption of salt, and avoid mouldy cereals or pulses(Node #351196)
Limit consumption of salt, and avoid mouldy cereals (grains) or pulses (legumes). The strongest evidence of methods of food preservation, processing, and preparation shows that salt and salt-preservered foods are probably a cause of stomach cancer, and that foods contaminated with aflatoxins are a cause of liver cancer.
8. Aim to meet nutritional needs through diet alone(Node #351197)Increasing the consumption of the relevant nutrients through the usual diet is preferred.
- The evidence shows that high-dose nutrient supplements can be protective or can cause cancer.
- The studies that demonstrate such effects do not relate to widespread use among the general population, in whom the balance of risks and benefits cannot confidently be predicted.
- A general recommendation to consume supplements for cancer prevention might have unexpected adverse effects.
Encourage physical activity in daily life(Node #348689)The Chief Medical Officer’s report (2011) recommends that adults aged 19-64 years undertake 150 minutes of moderate intensity physical activity per week in bouts of 10 minutes or more. [1]
More physical activity for kids within and beyond educational settings(Node #348687)
The introduction of compulsory physical education in schools is positive. However, greater promotion of physical activity outside of educational settings is also key to ensure any participation amongst pupils is not limited to school. Similarly, caution is needed to ensure that the promotion of competitive sport does not put off children less disposed to that sport. This could result in children either returning to or increasing their sedentary lifestyle.
British Heart Foundation recommends at least 60 minutes every day(Node #371560)
The British Heart Foundation recommends that to maintain their health, children take part in a minimum of 60 minutes of at least moderate intensity physical activity every day. This could include PE lessons, but also swimming, dancing, cycling, most other sports and brisk walking, as well as active play.
Quality and prevalence of physical activity in schools is variable(Node #371561)
The Ofsted Physical Education report published in February 2013 found that the physical aspect of physical education was not doing enough to tackle sedentary lifestyles amongst children and young people, with teachers often spending too much time talking and not enough time getting children moving.
Exercise benefits health and quality of life(Node #387192)
People live longer, feel better, function better, protect themselves from chronic diseases, and are generally happier when they’re active.
Exercise burns calories (Node #351149)
Exercise burns calories (and helps to achieve a better energy balance).
Exercise improves skeletal muscle insulin sensitivity(Node #351146)
Exercise makes the TCA cycle run faster(Node #351148)
...and detoxifies fructose, improving hepatic insulin sensitivity.
Exercise reduces stress, and resultant cortisol release(Node #351147)
Who should encourage physical activity in daily life?(Node #400663)
Better hydration(Node #348685)Government initiatives should include a greater focus on the importance of good hydration in weight management and health outcomes.
- By focusing primarily on healthy eating and food choices, existing guidance overlooks the undermining effect that poor hydration choices can have – and equally the benefits of good hydration choices such as water.
- The Eatwell plate, for example, could be usefully re-designed replacing soft drinks with water and incorporating reduced carbohydrates and a redefinition of fats.
The European Food Safety Agency (EFSA) recommends a total water intake of 2.0 litres a day for adult women and 2.5 litres a day for adult men under normal conditions. A greater intake is needed for those taking part in intense exercise, those who are pregnant or sick, or when the weather is particularly hot or humid.
While some fluid in the diet will come from food, the majority of this will come from drinks throughout the day. There are two related issues to consider:
(1) The importance of adequate fluid intake to maintain good health. Studies have proven that poor hydration can affect brain function. The benefits of an adequate fluid intake – particularly water – include maintaining a proper fluid balance within the body, maintaining normal bowel and kidney function, controlling hunger and maintaining an optimum cognitive ability. It is also an essential element of exercise.
- Yet it is not clear that the people of the UK are remaining properly hydrated. The initial findings of the UK Fluid IntakeStudy, published in 2012, found that 30 per cent of adults had inadequate intakes of fluid – as did more than 50 per cent of children. The study also found low levels of water consumption in relation to hot beverages and sugar sweetened beverages.
- These figures are backed by separate studies commissioned by the Department of Health and Food Standards Agency. This body of research has shown that children aged four to ten years typically consume 276ml of water per day and 620ml from other beverages (of which216ml was milk). Children and young people aged 11 to 18 years were found to consume 453ml of water per day and 680ml of other beverages, of which 150ml was milk.
(2) The contribution of fluid intake to calorie consumption. The initial findings of the UK Fluid Intake Study found that on average, sugar sweetened beverages provided 175 kcal per day of the calorie intake of children. This demonstrates the contribution that sugar sweetened beverages are making to rising levels of obesity.
- A study published by the British Journal of Nutrition in 2012 showed that, in 2008/09, beverages accounted for 21%,14% and 18% of daily energy intake for children aged 1.5–18 months, 4–18 years, and adults (19–64 years) respectively.
- The study noted that, since the 1990s, there had been an increased consumption of fruit juices (as well as reduced-fat milk) among children, while adults saw similar trends but additionally saw an increased consumption of alcohol. The study highlighted that using water as a substitute for caloric beverages may reduce overall energy intake.
- From a policy perspective, this leads to an imperative to acknowledge the contribution of sugar sweetened beverages to the diet and take steps to reduce this level. Many people will pay attention to what they eat, while overlooking the fact that sugar sweetened beverages can make a significant contribution to the amount of calories they consumer. In particular, there is a tendency to overlook the contribution that fruit juices and smoothies can make to sugar intake. While such drinks can provide one portion of the daily fruit and vegetable intake, the amount of sugar contained is similar to many carbonated beverages, the acidity can have a negative impact on dental health, and many of the juices lack the fibre content of fruit and vegetables, lessening the benefits to digestive health.
- Policy should focus on reducing the amount of sugar in beverages, reducing the amount of sugar sweetened beverages that are consumed, and promoting water or low calorie alternatives as the best way of remaining hydrated.
- Change4Life acknowledges this need, recommending that “all the family swapping to water, milk (ideally semi-skimmed, one per cent or skimmed), or sugar free drinks can really make a difference.” However, there is a need to make this more prominent in public health messaging.
Healthy traits spread dynamically through social networks(Node #351340)People’s traits – from happiness to obesity – can spread from person to person across the network of their social connections.
Create a strong, focused, coherent anti-obesity pressure group(Node #349038)
Evidence from the campaign against smoking suggests that a strong, focused, coherent anti-obesity pressure group may be essential to accomplishing sustainable systemic change.
Implement hard hitting campaigns, similar to those for anti-smoking(Node #348677)
Harder hitting campaigns, similar to those for anti-smoking, are required.
1. A sound scientific evidence base(Node #352274)
2. Authoritative reports from key organisations set out action needed(Node #352275)
3. A central point to lead advocacy and campaigning(Node #352276)
4. Coalition building(Node #352277)
5. Public support for policies and interventions(Node #352278)
Obesity is a more nuanced and complex problem than smoking(Node #371620)
The causal relationship between smoking and lung cancer is clear, specific and substantial and the solution (to stop smoking) is relatively simple, whereas the science underlying the causes of, and solutions to, obesity is more complex, uncertain and systemic.
Diversity and fragmentation of voices limits impact(Node #372583)
The multitude of organisations and voices campaigning on obesity adds to the complexity of the policy process and may become an impediment itself to change.
Lessons from Tobacco Control Policy(Node #352279)Policies are most effective if delivered as a package, and national policies are most effective if supported regional and local action.
From Linda Bauld [1]:
Although evidence on the health effects of smoking began accumulating over 200 years ago, it was not until the 1950s that any real attention was paid to this evidence. In 1950 five case control studies were published illustrating the link between lung cancer and smoking, including Doll and Bradford Hill‟s study. It took a further decade before the role of government in addressing smoking was acknowledged and a policy framework was proposed. In the UK, this framework was set out in the 1962 Royal College of Physician‟s report on Smoking and Health. This report set out recommendations for policy in six areas:
- the provision of public education on harm from smoking;
- restrictions on sales of tobacco to children;
- restrictions on advertising; restrictions on smoking in public places;
- increasing tobacco taxation; providing information on cigarette packs about tar and nicotine content; and,
- investigating the value of „anti-smoking clinics‟.
However, it would be almost half a decade later until all these measures were in place in the UK. Progress was achieved slowly. In 1965, television advertising of tobacco products was banned and in 1971 the first health warnings appeared on cigarette packs, followed by tar and nicotine yields in 1973. Also in the 1970s tobacco taxes were raised above inflation.
However, during the 1980s and early to mid 1990s relatively little policy progress took place. Instead, advocacy efforts escalated, led by Action on Smoking and Health (ASH) the tobacco control strategy established by the RCP in 1971. International tobacco control efforts also increased during this period and World No Tobacco Day was launched by the WHO in 1988. In 1993, Doll and Peto published results from the British Doctor‟s study that showed the extent of premature death due to smoking, with one in two smokers dying from smoking-related diseases13. This and other evidence persuaded the incoming New Labour government in 1997 to begin developing a package of policies that were outlined in the 1998 White Paper, Smoking Kills18. The policies in combination represented a comprehensive approach to tobacco control and included:
- An advertising ban (introduced in stages from 2002 to 2005)
- Tax increases (above the rate of inflation to 2001)
- Action on smuggling (increased from 2000)
- Mass media campaigns
- Enforcement of underage sales
- Better access to stop smoking medications
- The establishment of NHS stop smoking services
The policies set out in Smoking Kills did not include smokefree legislation but this was eventually introduced in England in 2007 following Scotland, Wales and Northern Ireland. Thus by 2007 all of the policies originally recommended in the RCP report were in place. Further progress, including the introduction of visual health warnings on packs (2008), raising the age of sale from 16 to 18 (2007) and the commitment to a point of sale display and vending machine ban (2009, not yet implemented) was made more recently.
What factors explain this progress, particularly in the past 10-15 years?
Key ingredients include:
- A sound scientific evidence base
- Authoritative reports from key organisations setting out action needed
- A central point to lead advocacy and campaigning
- Coalition building Public support for policies and interventions
- Political support for policies and interventions
The evidence for tobacco control began with studies on the impact of smoking but now includes a considerable body of research setting the rationale for, and impact of particular policies and interventions. This evidence has been invaluable in persuading planners and policy-makers to invest in tobacco control measures.
Key organisations such as the RCP and the British Medical Association (BMA) have used this evidence to produce authoritative reports that have made the case for policies and interventions, underpinned by international developments such as the implementation of the World Health Organisation Framework Convention on Tobacco Control (FCTC) from 2005.
The existence of ASH as a central point for advocacy and campaigning has also been crucial, and ASH has been able to act as a focus for coalition building. The Smokefree Action Coalition, for example (with its roots in earlier coalitions, this partnership was formed to advocate for smokefree legislation) is centred around ASH but includes a wide range of charities and other organisations that are advocates for tobacco control.
Their actions combined with the evidence (often communicated through mass media campaigns) have helped to shape public opinion in favour of measures to address smoking. These measures have built up over time, assisting in denormalising tobacco use which has further contributed to public support.
New Labour‟s support for tobacco control undoubtedly contributed to the rapid progress observed in reducing smoking between 1998 and 2008 in particular - a steady decrease of 0.5% each year. It remains to be seen to what extent the change in government at Westminister in 2010 will affect tobacco control, and smoking prevalence, in the longer term.
Improve food labelling(Node #352380)
Major food manufacturers and supermarkets should agree in the next year a unified system of traffic light food labelling (to be based on percentage of calories for men, women, children and adolescents) and visible calorie indicators for restaurants, especially fast food outlets.
Make environmental indicators relevant for obesity policy(Node #352824)
Making environmental indicators (e.g. food miles) meaningful for obesity policy.
Support honest consumer information(Node #352836)
Types of labeling intervention(Node #366471)Cost-effective interventions to reduce obesity in the UK
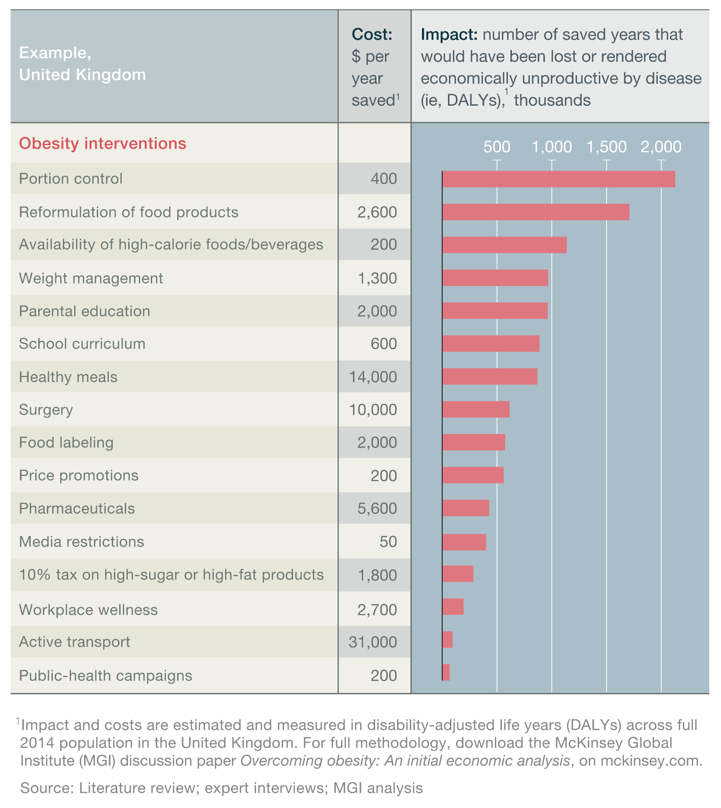
Aggregate basket calorie labeling: retailers(Node #366514)
Retailers provide traffic-light rating of basket contents at checkout.
Aggregate meal calorie labeling: restaurants(Node #366513)
Fast-food restaurants provide aggregated nutritional content and traffic-light labels at checkout.
Aggregate meal calorie labeling: workplace(Node #366512)
Employers provide aggregated nutritional content and traffic-light labels at checkout.
Calorie/nutrition “engaging” labeling on package: regulated(Node #366505)
Government mandates front-of-pack “engaging” format nutritional information (e.g., traffic-light labels) on all packaged foods.
Calorie/nutrition “engaging” labeling on package: self-regulated(Node #366515)
Industry self-regulates front-of-pack and “engaging” format nutritional information (e.g., traffic-light labels) on all packaged foods.
Calorie/nutrition “plain” labeling on package: regulated(Node #366503)
Government mandates nutritional labeling on all packaged foods.
Calorie/nutrition “plain” labeling on package: self-regulated(Node #366504)
Industry self-regulates nutritional labeling on all packaged foods.
Nutrition “engaging” labeling: workplace(Node #366511)
Employers provide “engaging” workplace canteen nutritional labeling (e.g., traffic-light labels).
Nutrition “plain” labeling: workplace(Node #366510)
Employers provide workplace canteen nutritional labeling.
Nutrition labeling in restaurants: regulated(Node #366508)
Government mandates labeling on menus and shelf choices in fast-food restaurants .
Nutrition labeling in restaurants: self-regulated(Node #366509)
Fast-food restaurants label menus and make shelf choices.
Portion-size “engaging” labeling on package: regulated(Node #366506)
Government mandates “engaging” portions information on each package in a clearly communicated way.
Portion-size “engaging” labeling on package: self-regulated(Node #366507)
Industry self-regulates “engaging” portions information on the front of the package in a clearly communicated way.
Calorie labels on food do more harm than good(Node #371477)
Evidence suggests that calorie counts are ineffective and potentially counter-productive for certain consumers.
false labels(Node #657246)
labels may be false
Align the school curriculum with obesity, nutrition and activity goals(Node #366479)The Cochrane Review [4] concluded:
We found strong evidence to support beneficial effects of child obesity prevention programmes on BMI, particularly for programmes targeted to children aged six to 12 years. However, given the unexplained heterogeneity and the likelihood of small study bias, these findings must be interpreted cautiously. A broad range of programme components were used in these studies and whilst it is not possible to distinguish which of these components contributed most to the beneficial effects observed, our synthesis indicates the following to be promising policies and strategies:
· school curriculum that includes healthy eating, physical activity and body image
· increased sessions for physical activity and the development of fundamental movement skills throughout the school week
· improvements in nutritional quality of the food supply in schools
· environments and cultural practices that support children eating healthier foods and being active throughout each day
· support for teachers and other staff to implement health promotion strategies and activities (e.g. professional development, capacity building activities)
· parent support and home activities that encourage children to be more active, eat more nutritious foods and spend less time in screen based activities
However, study and evaluation designs need to be strengthened, and reporting extended to capture process and implementation factors, outcomes in relation to measures of equity, longer term outcomes, potential harms and costs.
Childhood obesity prevention research must now move towards identifying how effective intervention components can be embedded within health, education and care systems and achieve long term sustainable impacts.
Cost-effective interventions to reduce obesity in the UK
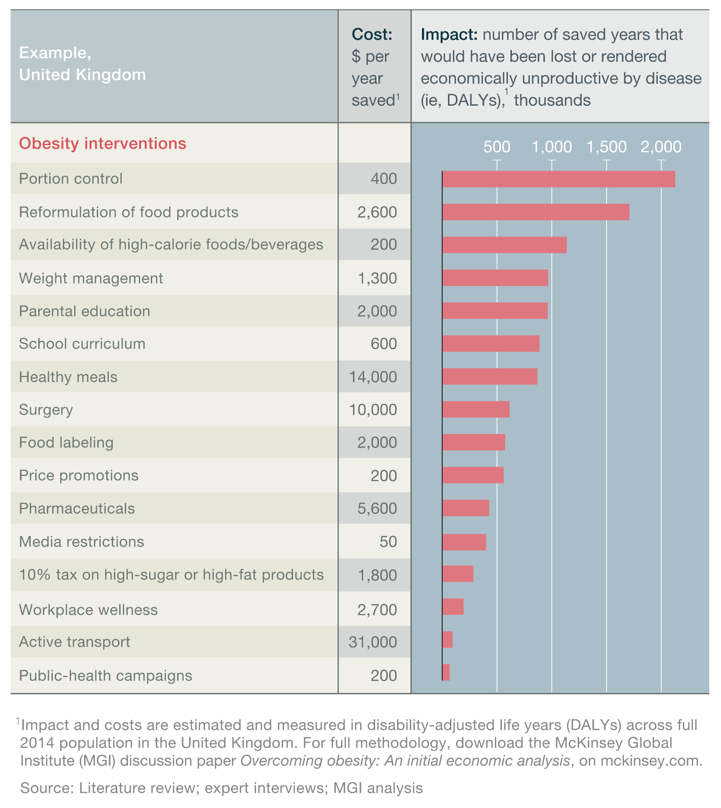
Help educate ‘taste’ to be more discriminatory (Node #352787)
School curriculum includes nutritional-health education: regulated(Node #366537)
Schools include or increase the amount of nutritional-health education.
School curriculum mandates physical activity: regulated(Node #366536)
Schools mandate or increase the amount of physical activity in the curriculum.
School temporary diet and exercise programs(Node #366535)
Schools provide short-term intensive nutritional education or exercise programs.
Support media analysis in schools and commerce-free schools(Node #352790)
Teach the joy of eating ‘excess’ only as feast day(Node #352838)
Teach the joy of eating ‘excess’ only as feast day rather than everyday experience.
Different children have different contexts and needs (Node #371558)
Policy measures – and the messaging associated with them – need to be sufficiently flexible and intelligent across different contexts to reflect the fact that children's experiences vary widely and that many children are already physically active.
Unintended consequences of anti-obesity messages to children(Node #371557)
Research suggests that the anti-obesity health messages targeted at students can have unintended and deleterious consequences for the children.
Improve parental education(Node #366473)Cost-effective interventions to reduce obesity in the UK
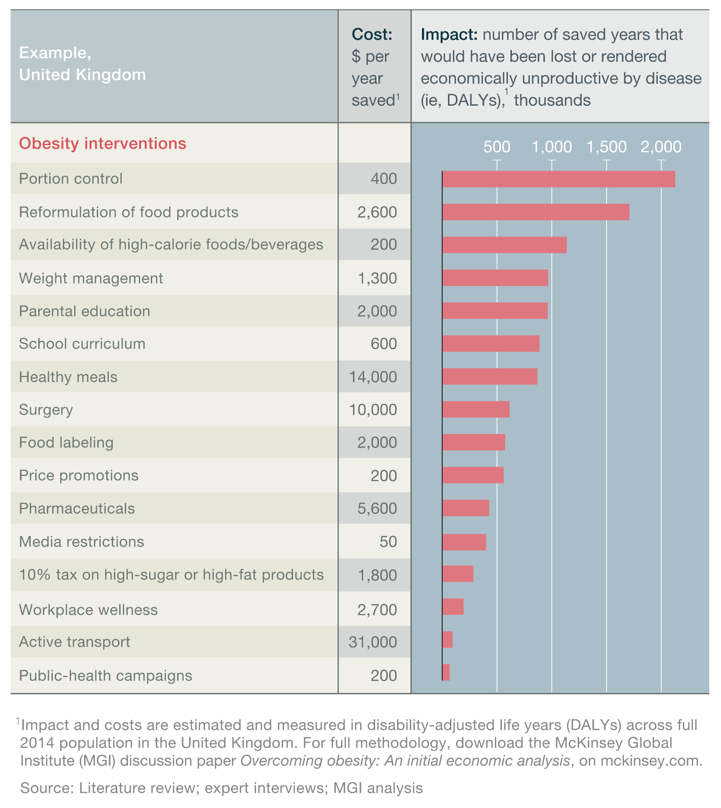
Avoid using unhealthy foods as rewards for children(Node #371450)
Encourage responsibility for long-term benefit not short-term peace(Node #352845)
Help to define parental responsibility for long-term benefit rather short-term ‘peace’
Increase support for new parents(Node #352375)
The current expansion of the health visitor workforce in England should be accompanied by 'skilling up' the wider early years workforce to deliver basic food preparation skills to new mothers and fathers, and to guide appropriate food choices which will ensure nutritionally balanced meals, encourage breastfeeding and use existing guidance in the Personal Child Health Record as a tool to support this.
Early years’ intervention is vital to reducing health inequalities(Node #371449)
Parental education: preschool-age children(Node #366519)
Government authorities provide educational program (e.g., 12-week course) to parents of preschool-age children covering nutrition and parental feeding styles, and providing opportunities for physical activity
Parental education: schoolchildren(Node #366520)
Government authorities provide educational program (e.g., 12-week course) to parents of preschool-age children covering nutrition and parental feeding styles, and providing opportunities for physical activity.
Use food as an affirmative social engagement, e.g. eating together (Node #352843)
Encourage parents to use food as an affirmative social engagement, e.g. eating together.
Strengthen the evidence base on obesity(Node #352727)
Develop a scientific systems approach to food and nutrition policies(Node #368066)
Developing a scientific framework for a systems approach to food and nutrition policies.
Improve the evidence base for adoption of healthier dietary behaviour(Node #368065)
Provide a framework to design, monitor and evaluate policies(Node #368067)
Understand the feasibility / impacts of individualised, healthy diets(Node #368068)
Who should improve public education & literacy on obesity & nutrition(Node #352724)
Who should improve public education, literacy and actions on obesity and nutrition and health?
Reshape the food environment to encourage healthier eating patterns(Node #366482)Create an environment that better suits our biology and supports us in developing and sustaining healthy eating and activity habits. Aim to amplify patterns that promote and support healthy eating patterns and damp patterns that encourage unhealthy eating patterns.
Cost-effective interventions to reduce obesity in the UK
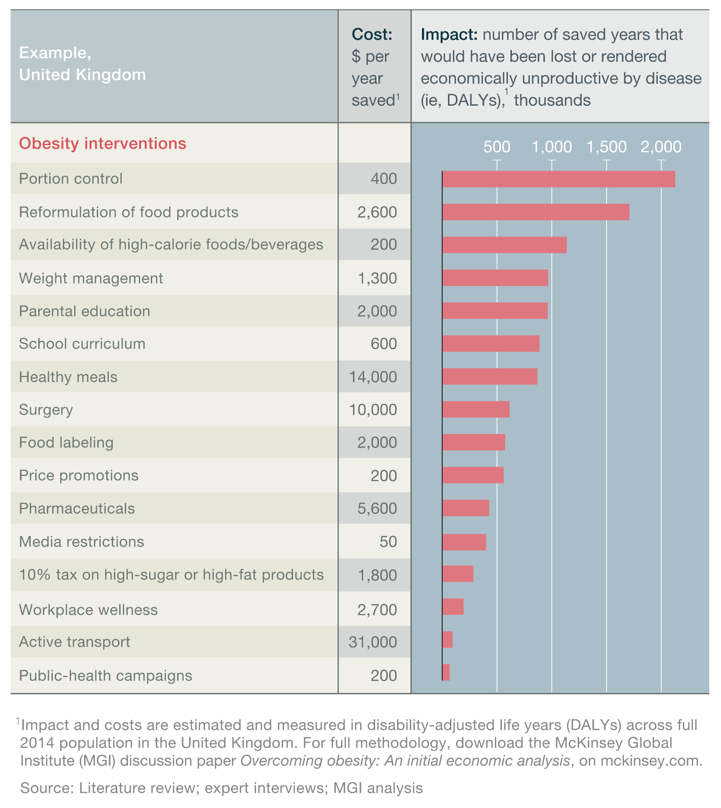
Reduce portion sizes(Node #366475)Food producers, restaurants and workplace canteens should reduce average portion sizes (including removing extra-large "super-size" single-serve portions from packaged food ranges and menus).
Cost-effective interventions to reduce obesity in the UK
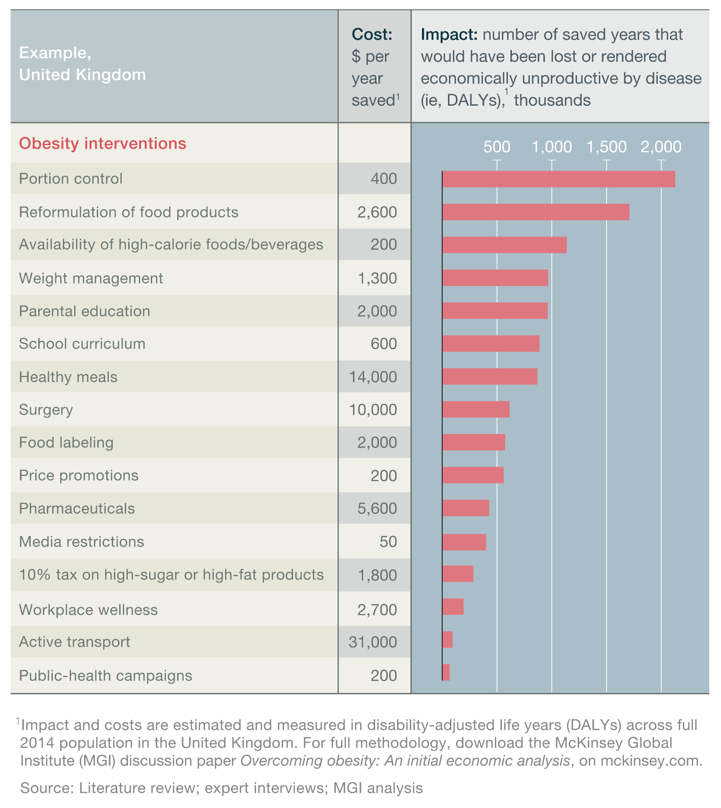
Food producers reduce average portion sizes(Node #366523)
High-calorie beverage producers reduce average portion sizes(Node #366526)
Beverage producers reduce average portion sizes of high-calorie beverages.
Restaurants reduce average portion sizes(Node #366524)
Restaurants reduce average portion size of meals and snacks.
Schools reduce average portion sizes offered to children(Node #371773)
Workplace canteens reduce average portion sizes(Node #366525)
Employers reduce average portion size of foods in workplace canteens.
How to regulate the portion sizes of food eaten at home?(Node #371533)
The average energy intake from eating out accounts for only around 10 per cent of total energy intake (with the total energy intake per person estimated to be an average of 2,192 kcal per person per day versus an approximate energy intake from eating out of 220 kcal per person per day).
Encourage the perception that large portion sizes are anti social(Node #371534)
Encouraging the perception that large portion sizes are anti social might help to reduce the portion sizes that people prepare and consume at home.
Anti-social campaign worked well against smoking(Node #371535)
The well-organized and sustained campaign to portray smoking as an anti-social activity appears to have played a significant role in the reduction of smoking (and therefore might play a similarly effective role in reducing the portion sizes and prepared and consumed at home).
Eating out accounts for only around 10% of average energy intake(Node #371568)
The average energy intake from eating out accounts for only around 10 per cent of total energy intake. The total energy intake per person was an average of 2192 kcal per person per day in 2012, and the energy intake from eating out was 220 kcal per person per day in 2013.
Reformulate food and beverages(Node #366478)Industry produces and delivers food and beverages with an improved nutritional profile.
Cost-effective interventions to reduce obesity in the UK
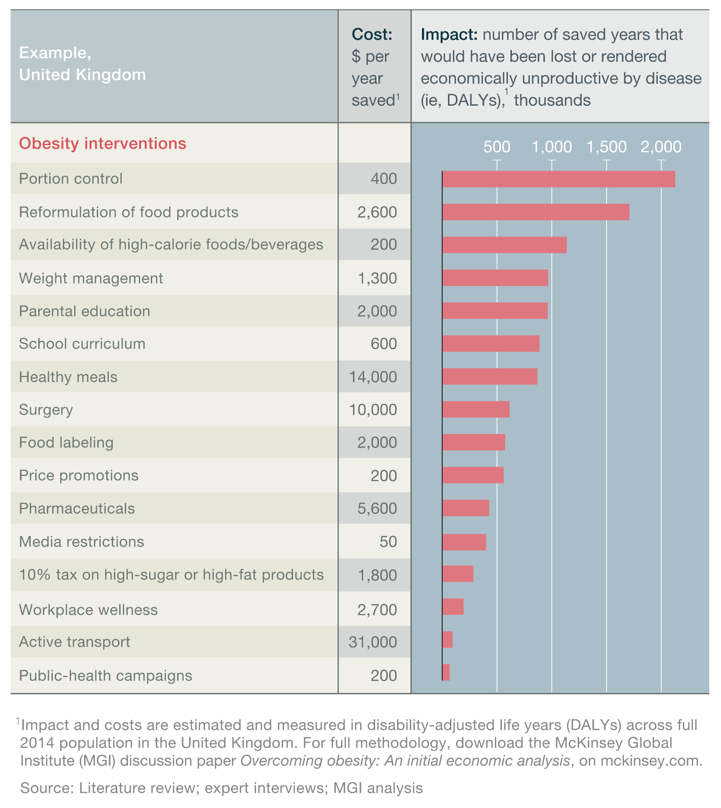
New “better for you” products(Node #366531)
Introducing new product ranges with improved nutritional profile, and advertised as such.
Stealth product reformulation: beverages(Node #366533)
Beverage producers deliver small, incremental reduction in the caloric content of beverages that consumers do not notice.
Stealth product reformulation: food(Node #366532)
Food producers deliver small, incremental changes to formulation of food products (e.g., reduction in sugar) that consumers do not notice.
Stealth product reformulation: restaurants(Node #366534)
Fast-food retailers deliver small, incremental changes in the formulation of food products that consumers do not notice.
Market unhealthier food responsibly(Node #352737)
Restrict junk food advertising(Node #352378)
Ban television advertisements of foods high in saturated fats, sugar and salt before 9pm, and seek agreement with commercial broadcasters not to advertise these foods on internet ‘on-demand’ services. [2]
Types of media restrictions(Node #366472)Cost-effective interventions to reduce obesity in the UK
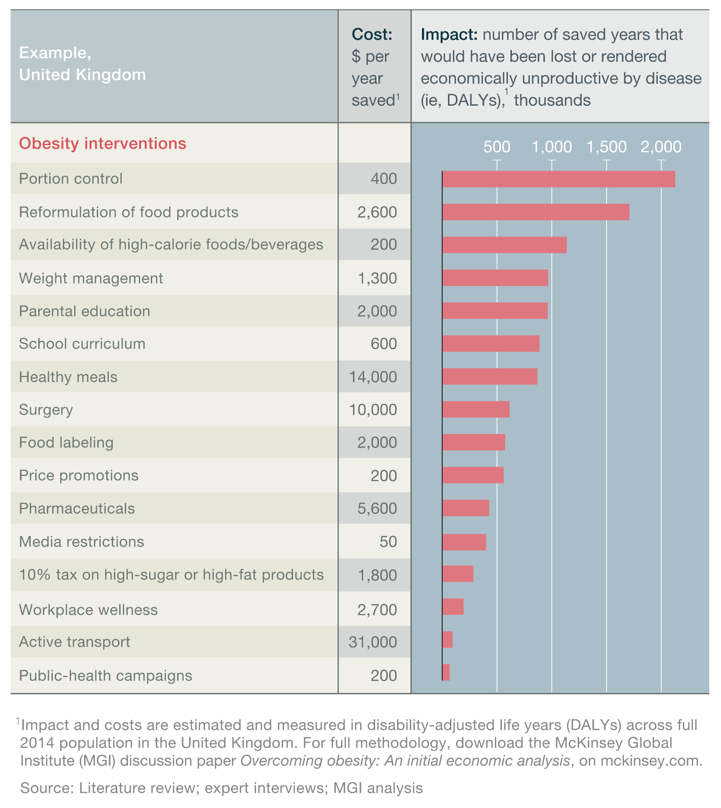
Media restriction on high-calorie advertising on TV: regulated(Node #366517)
Government restricts advertising of high-calorie foods on TV from 6 a.m. to 9 p.m.
Media restriction on high-calorie food advertising: regulated(Node #366516)
Government restricts advertising of high-calorie foods on all advertising supports.
Media restriction: self-regulated(Node #366518)
Food and beverage industry voluntary restricts high-calorie food advertising (e.g., to children).
Accept restrictions on food marketing(Node #352833)
Accepting restrictions on the commoditization of relationships in food marketing.
Agreeing not to target children(Node #352835)
Adopt a precautionary principle for the marketing of foods to children.
Make high-calorie food and drink less prominent(Node #366470)Cost-effective interventions to reduce obesity in the UK
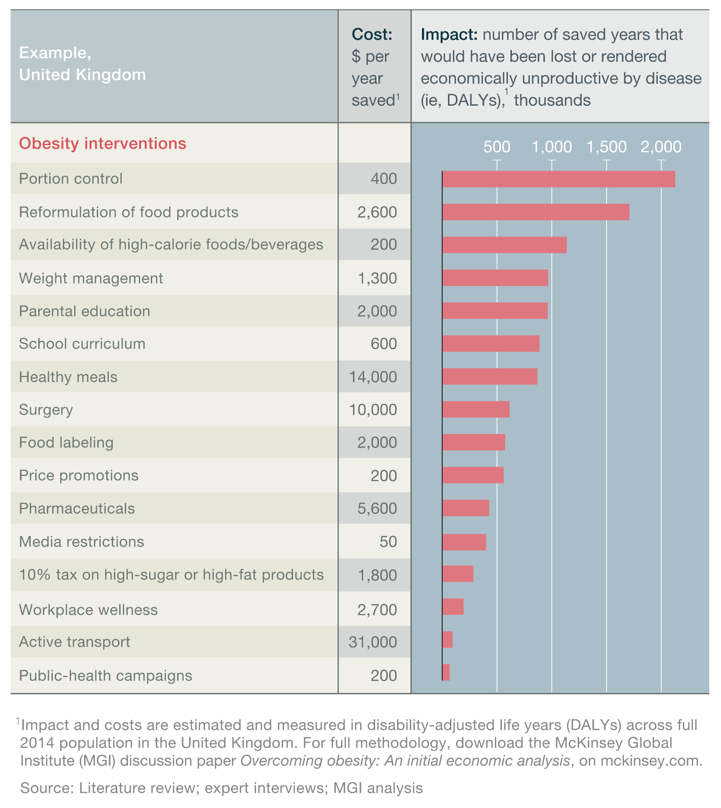
Reduce fast food outlets near schools(Node #352377)Public Health England should, in its first 18 months of operation, undertake an audit of local authority licensing and catering arrangements with the intention of developing formal recommendations on reducing the proximity of fast food outlets to schools, colleges, leisure centres and other places where children gather.
"Using the example of school food we were told of the anomaly that existed within many local authority boroughs where licencing practices mean councils actually end up undermining their own efforts in the schools by allowing the expansion of outlets which sell food that is high in salt, sugar and saturated fats which in effect pull children away from healthy eating.
Many times in the inquiry we heard about the valiant secondary school doing its utmost to put on high quality, affordable lunches for their pupils but being undercut by the local chip and chicken shop with its ‘pocket money’ prices. Older children understandably want the freedom of going off site at lunchtime but it is extraordinary that the local authority which is trying to encourage a child to have a healthy lifestyle in school allows an environment which nudges them to do precisely the reverse.
We were told that many local authorities do not exercise the appropriate controls which can be placed on mobile food units which results in the paradox that burger vans, once licenced, are in effect free to pitch up wherever they like so long as they do not infringe traffic regulations.
Some local authorities have woken up to this and are taking decisive action to create a more level playing field. Councils such as Waltham Forest and Tower Hamlets and cities like Liverpool have introduced strategies to reduce obesity which include addressing obvious inconsistencies such as this."
Reduced access to high-calorie food in schools: regulated(Node #366498)
Government bans vending machines and snack shops in schools.
Reduced access to high-calorie food in schools: self-regulated(Node #366499)
Schools voluntarily ban vending machines and snack shops.
Reduced access to high-calorie food in the workplace(Node #366500)
Employers remove vending machines and easy access to high-calorie foods.
School canteen layout(Node #366501)
Schools place healthier canteen areas (e.g., vegetables, fruit, and salad) more prominently.
Supermarket layout: prominence(Node #366497)
Grocery retailers allocate greater prominence (aisle ends, checkout counters, store entry) to healthier products.
Supermarket layout: space(Node #366496)
Grocery retailers allocate greater share of space to healthier products and categories .
Workplace canteen layout(Node #366502)
Employers place healthier canteen areas (e.g., vegetables, fruit, and salad) more prominently.
Promote wholesome food to all, especially to low-income groups(Node #352831)
Promoting good, wholesome food to all, but especially to low-income social groups.
Supermarket targeted promotions(Node #366494)
Grocery retailers promote healthy eating through campaigns and recipes.
Encourage healthier meals in the workplace(Node #366469)Cost-effective interventions to reduce obesity in the UK
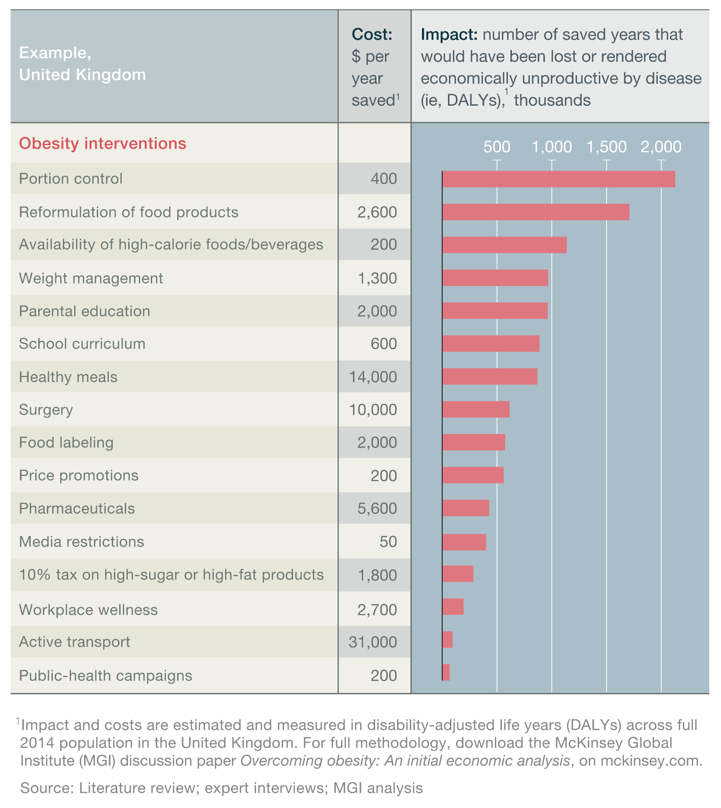
Free healthy meals in the workplace(Node #366493)
Employers provide free healthy meals.
Lower-calorie options in the workplace(Node #366495)
Employers introduce healthy options in canteens but do not remove existing options.
Improve nutritional standards for food in hospitals(Node #352374)Introduce food-based standards—in line with those put in place for schools in England in 2006—in all UK hospitals in the next 18 months; with commissioners working with a delivery agent similar to the Children’s Food Trust to put these measures into place.
From Measuring Up: [1]
"In the NHS we have begun to realise that the environment in which we treat our patients can sometimes be as critical as the way in which we treat them. It is perplexing therefore to walk into a hospital canteen, a place where we should be sending strong signals about good nutrition, to find that the food provision is unhealthy and fails to meet the same requirements that we expect, for example, in schools. It is even more astonishing that in many hospital receptions patients pass by high-street fast food franchises or vending machines selling confectionery, sugary drinks and crisps. If the NHS is to send out a message that it takes the obesity crisis seriously, then it needs at the very least to avoid providing the same obesogenic environment as the high street and make sure that patients and staff alike are offered healthy and nutritious meal choices.
The sustainable food alliance Sustain has long campaigned on this issue and point out that while schools and prisons have food standards, to improve the health of children and prisoners, hospitals do not. [2] In the same manner that smoking was banned in hospitals and healthcare settings, we believe that staff and patients should be given healthy catering options.
There are many ways to present nutritionally balanced meals which are also attractive and affordable. Indeed, we were pleased during the writing of this report that our recommendation has already been partially adopted by the Department of Health in England with the announcement of new ‘principles’ for hospital food which will be evaluated by teams of assessors, half of whom must be patients.
However, these ‘principles’ are vague and voluntary and may by themselves have little impact. We think that mandatory standards may prove necessary. We hope that the health departments in the other home nations take on the challenge, and that mandatory standards for food are introduced in hospitals across the UK."
Improve nutritional standards in schools(Node #352376)
The existing mandatory food- and nutrient-based standards in England should be applied to all schools including free schools and academies. This should be accompanied by a new statutory requirement on all schools to provide food skills, including cooking, and growing – alongside a sound theoretical understanding of the long-term effects of food on health and the environment.
Apply mandatory food- and nutrient-based standards to all schools(Node #371803)
The existing mandatory food- and nutrient-based standards in England should be applied to all schools including free schools and academies.
Free compulsory school meals for all(Node #366491)
Government provides free compulsory school meals and improves health quality
Require all schools to provide food skills and understanding(Node #371804)
Introduce a statutory requirement on all schools to provide food skills, including cooking, and growing, alongside a sound theoretical understanding of the long-term effects of food on health and the environment.
Subsidized compulsory school meals for all(Node #366492)
Government subsidizes compulsory school meals and improves health quality.
Benefits of healthy behavioural change will ripple across lifetimes(Node #371801)
Improved engagement and concentration(Node #371802)
Improving the food and dining environment for children increases the likelihood that children will be engaged and concentrate in afternoon lessons.
Eliminate food deserts(Node #366546)
A ‘food desert’ is an area in which there is limited local availability of healthy food.
Who should reshape the food environment?(Node #400391)
Who should reshape the food environment to encourage healthier eating patterns?
Shape the physical environment to encourage physical activity(Node #366828)Adults have been recommended to take part in 150 minutes of moderate intensity activity every week – but evidence suggests that in England only one in 20 people meet this recommended level of activity.
Encourage active transport (walking and cycling)(Node #366467)Government authorities redesign urban planning to facilitate and encourage walking and cycling.
Cost-effective interventions to reduce obesity in the UK
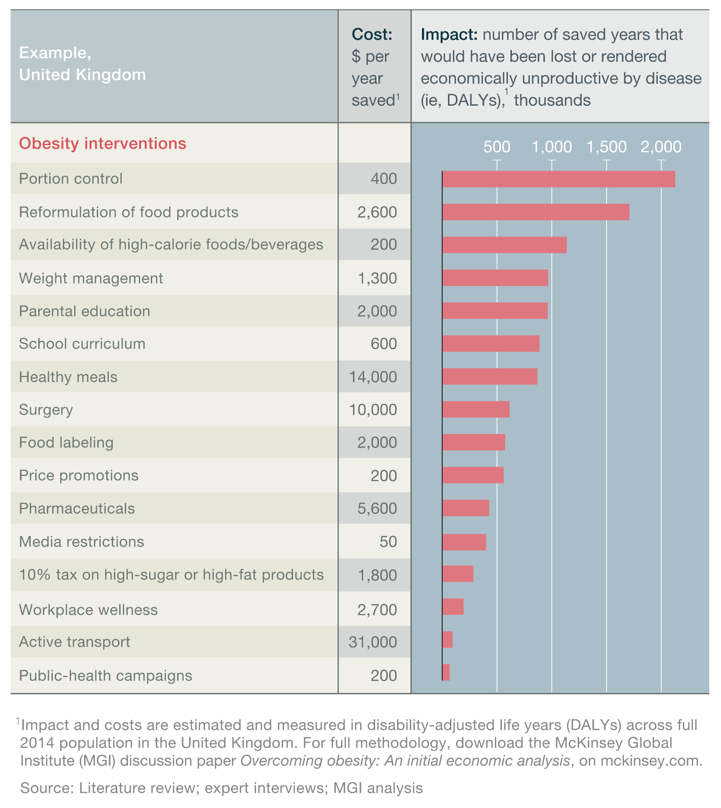
Make people feel secure to walk or bicycle to work/school/leisure(Node #352773)
Enable children to play in public places, streets and parks (Node #352840)
Get out of homes more to reclaim civic space(Node #352841)
Make it easier for people to walk rather than drive to shops(Node #352828)
Offer fewer parking spaces for cars(Node #352842)
Reduces reliance on fossil fuels(Node #352821)
Encourage physical activity in daily life helps to reduce society's reliance on fossil fuels.
Mandatory health impact assessments for local planning decisions(Node #352381)
Local authority planning decisions should be subject to a mandatory health impact assessment, which would evaluate their potential impact upon the populations’ health.
Use planning functions to routinize physical activity (Node #352776)
Improve community sports facilities and programs(Node #366545)
Increase public access to community sports facilities and programs.
Invest in school physical exercise facilities(Node #366544)
Government authorities/schools invest in higher-quality physical exercise facilities.
Protect and increase green spaces(Node #371774)
Public Health England should provide guidance to Directors of Public Health in working with Local Authorities to encourage them to protect or increase green spaces.
Who should shape the physical environment?(Node #400392)
Who should shape the physical environment to encourage physical activity?
Develop a coherent fiscal, regulatory and governance framework(Node #366827)
Take every opportunity, iteratively over time, to bring the public fiscal, regulatory and governance framework into alignment with public health goals on obesity. Use taxes, subsidies, targets and pricing signals to incentivise change in behaviour, supply and consumption by aligning measures with the health properties of food and drink and behaviour—and seek, wherever practical, to amplify positive patterns that are aligned with the policy goals and damp those that pull against.
Use taxation and subsidies to encourage healthier food choices(Node #352826)
Use taxation to encourage healthier food choices(Node #351219)
Use taxation to drive price increases on unhealthy types of food or nutrient.
Tax sugary beverages(Node #352478)
Introduce a tax on sugary soft drinks (i.e. levy the tax on the final products)
How much sugar needs to be added before the drink is taxed?(Node #351231)
Pilot a 20%+ tax on all sugary, soft drinks for 1 year(Node #352379)
For an initial one year, a duty should be piloted on all sugary soft drinks, increasing the price by at least 20%. This would be an experimental measure, looking at price elasticity, substitution effects, and to what extent it impacts upon consumption patterns and producer/retailer responses.
Tax all sugar-sweetened drinks(Node #351229)
Tax all sweetened drinks(Node #351230)
Tax rate would need to be at least 20% to be effective(Node #351233)
Excise duty on unhealthy raw ingredients(Node #352476)
Use excise duty – e.g. calculated on the basis of the amount of sugar, salt or saturated fat that a foodstuff contains – as a supply side measure shape food production.
Extra cost becomes a demand side pricing signal if passed to consumers(Node #368615)
Make food acquisition costs reflect environmental externalities (Node #352820)
Reward food manufacturers for healthier reformulation(Node #368614)
Reformulate VAT on food, such that VAT is levied on unhealthy foods(Node #368238)
Implement valued added tax mechanisms to make foods high in sugar and saturated fat more expensive
VAT are measures more likely to raise revenue than change behaviour(Node #368616)
Evidence from France and Hungary suggests that the tax increases would act as revenue raisers rather than for health benefits, as the rate of tax was too low to impact sufficiently on consumption.
Health related food and drink taxes could improve health(Node #351223)
Taxes on food and drink would be ineffective(Node #351225)
Taxes on food and drink would be regressive(Node #351224)The Institute for Fiscal Studies concluded that a "fat tax" would probably be regressive, costing the poor relatively more than the rich; because consumption of fat and other ‘bad’ nutrients does not differ much across the income distribution.
- For the hypothetical tax we model, the poorest households lose around seven times more, as a proportion of income, than the richest households do, on the assumption that there is no behavioural change.
- The regressivity of a ‘fat tax’ is likely to hold no matter how the tax is implemented – whether on fat content, on calories or just attached at a particular rate to certain foods.
Taxes on food and drink would damage the food and drink industry(Node #351226)
Taxes on food and drink would result in job losses(Node #351227)
Examples of taxation on unhealthy food and drinks(Node #351234)
Denmark has introduced a fat tax(Node #351238)
Denmark targeted its attack on saturated fats, unveiling a levy of €2.41 per kilogram of saturated fat used in the production of a particular food. The effect is to levy a heavier tax on higher fat foods, such as hamburgers or butter. The tax kicks in when the saturated fat content of a food product tops 2.3%.
France has introduced a tax on sweetened drinks(Node #351240)
France has introduced a new €0.036 per litre tax on sweetened drinks. Sugar-free soft drinks, water and unsweetened fruit juices escape the levy.
Hungary has taxes on a range of unhealthy foods(Node #351239)
Hungary has introduced taxes on foods with high fat, sugar, salt and caffeine content, as well as increasing its tariffs on soda and alcohol. A levy has been added on soft drinks of €0.016 per litre, €0.33 per kilogram for prepackaged sweetened products, €0.67 per kilogram for salty snacks, and €0.84 per litre for energy drinks.
Use subsidies to encourage healthier choices(Node #352778)Government food subsidies should promote healthier food ranges (eg fruit/vegetables).
Trends in fruit and vegetable purchases measured as portions
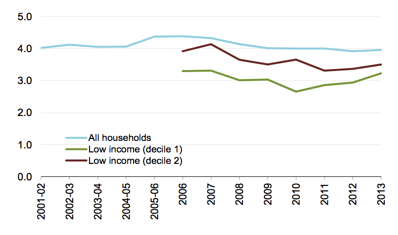
Source: DEFRA
- On average, all households purchased 4.0 portions of fruit and vegetables per person per day in 2013.
- Lower income households (deciles 1 and 2) have consistently purchased smaller quantities of fruit and vegetables, although both have increased in the last two years.
- Income decile 1 households purchased 3.2 portions of fruit and vegetables per person per day in 2012.
Reduce existing subsidies on unhealthy food commodities and products(Node #352830)
Government reduces existing subsidies on fat, meat and dairy products and food commodities that drive prices (e.g., processed foods such as corn, sugar, and palm oil).
Reform the Common Agricultural Policy to promote health(Node #370192)
Health benefits should be an explicit, legitimate outcome of CAP spending, and CAP reform offers a significant opportunity to address the burden of cardiovascular disease (CVD) by addressing 'distortions' in relation to certain food prices and production processes which potentially increase the burden of disease. [1]
Ensure CAP spending takes account of its impact on CVD risk factors(Node #371806)
The European Commission's impact assessment procedure, part of its strategic planning and programming cycle, should include cardiovascular health and other health issues, so that CAP spending takes adequate account of its potential impact on CVD risk factors and is used in a way that optimises the public health outcomes. [1]
Include health promotion and disease reduction in CAP's public goods(Node #371805)
Formal recognition of health a public good will ensure that promoting health and reducing disease is made an explicit part of the CAP's 'public goods' and that the CAP, and the associated funding, works to promote the wellbeing of EU citizens. [1]
Pillar Two funds should encourage production of healthier foods(Node #371807)
Future 'pillar two' funds should reward or encourage the production of highly nutritious foods such as fruit, vegetables, whole grains and leaner meats, and payments under 'pillar one' should be phased out progressively so that all payments fall under 'pillar two'. [1]
Use agricultural subsidies to make fresh fruit and vegetables cheaper(Node #352482)
Food stamps to help low-income people buy fruit and vegetables(Node #366541)
Government provides personal subsidies (e.g., food stamps for low-income individuals for sole use on certain healthy food types).
Offer tax breaks to firms that incentivise employee health(Node #373021)
Offer tax breaks to employers who provide effective NICE-certified workplace health programmes for employees.
Withdraw sickness benefit from claimants who refuse obesity treatment(Node #387262)
People who claim sickness benefit – incapacity benefit, severe disablement allowance, or employment and support allowance – because of obesity could have this money withdrawn if they refuse treatment for their obesity. [1]
How to address cases in which suggested treatment is unsuccessful?(Node #387265)
What would happen in cases in which individuals try but fail to lose weight on the required programmes. And how will “trying” be determined? [1]
Benefits of diet and lifestyle measures often restricted and transient(Node #387263)
Diet and lifestyle interventions have restricted, often transient, benefits due to biological adaptations, that act to sustain high bodyweight.
More staff would be required to deliver and monitor these services(Node #387269)
Although government funding already supports some diet and lifestyle programmes for people with obesity, more funding would be needed to recruit and train staff to deliver these services and to monitor attendance and participation.
Requiring bariatric surgery would be unethical(Node #387264)
The only treatment for obesity that has been proven to be successful for substantial long-term weight loss and improved quality of life in a high proportion of people is bariatric surgery; however, requiring people to undergo a major surgical procedure as a condition of receiving benefits seems far from ethical.
Only 1,780 people claiming sickness benefits due to obesity in May '14(Node #387268)
The number of people claiming sickness benefits with obesity as the primary reason for the claim is actually very small (only 1780 people as of May, 2014). [1], [2]
Align public food procurement and catering with public health goals(Node #352779)Public sector organisations are estimated to provide around one in three meals eaten outside the home, so the government can further its public health goals, and model the behaviour it desires to see others adopt, by setting and paying for high standards of public sector catering.
Build partnerships with industry(Node #351048)
Work with industry to make healthier products and to market them more responsibly – and where practical and appropriate encourage voluntary self-regulation by industry.
Adopt a precautionary principle(Node #351053)
A precautionary principle should be adopted given the uncertainty that the inherent conflicts of interest with industry can be reconciled, and the consequences of being wrong if they cannot.
Align companies’ success with consumer health (Node #352832)
Apply best advertising and marketing strategies to healthier choices(Node #386176)Apply the best and most creative strategies from the advertising and marketing world to healthier choices.
Place onus of proof on industry(Node #368618)
The onus should be on companies to demonstrate rigorously and independently that the self-regulatory measures and/or private–public partnerships are improving public health as well as private profit. Where this is found to be case, the specific methods should be extended and replicated.
Voluntary price increases of high-calorie food and beverages(Node #366476)Food producers/retailers voluntarily increase price of high-calorie food and beverages.
Cost-effective interventions to reduce obesity in the UK
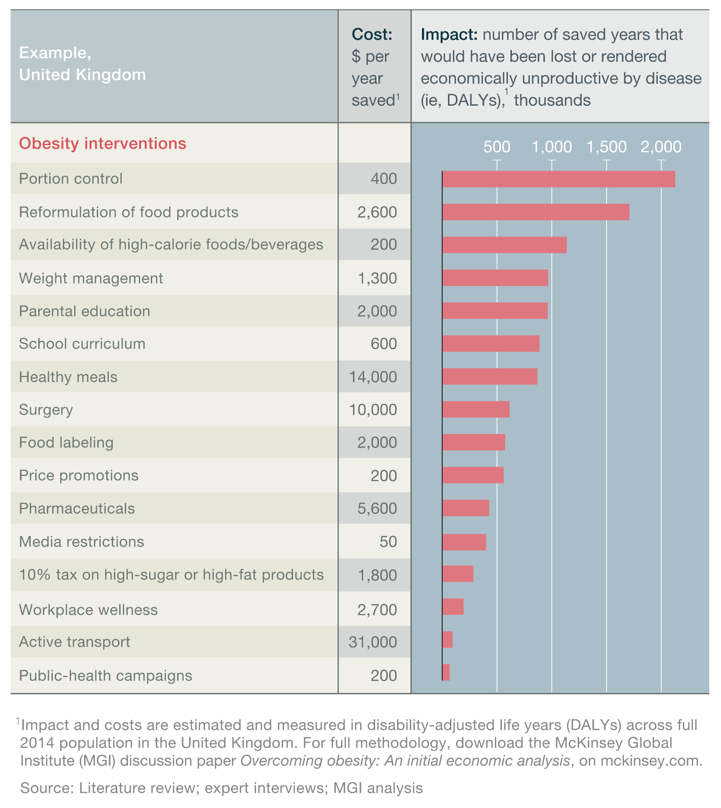
Voluntary reduction in promotions of high-calorie food and beverages(Node #366528)
Retailers and producers restrict promotional activity (e.g., two-for-one) of high-calorie food and beverages.
Partnerships strengthen the voices for change within companies(Node #372539)
Government partnerships with industry help to strengthen the voices, role and position of the advocates for change within the companies.
Self-regulation and public-private partnerships have worked before(Node #371073)
Industry self-regulation and public-private partnerships have worked successfully in the public interest in a number of cases.
Salt-reduction by reformulation in the UK(Node #371165)The UK initiated a nationwide salt reduction programme in 2003/2004. The programme has been successful and resulted in a 15% reduction in population salt intake by 2011.
Factors that contributed the success of the voluntary salt-reduction programme, included:
(1) The programme provided a level playing field.
(2) The reformulation process was slow and unobtrusive; so taste receptors could adjust and there was no rejection of the reformulation by the public.
(3) The voluntary policy was supported with a clear and transparent monitoring programme and strong enforcement (thanks, in part, to the role played by the Food Standards Agency).
(4) Continuous media exposure of the issue.

Source: Feng J He, Sonia Pombo-Rodrigues, Graham A MacGregor, BMJ
Folate fortification of flour and bread products(Node #371077)
Folate fortification of flour and bread products to help reduce rates of neural tube defects is an example of the way in which public-private collaborations with the food industry can boost public health.
Pharmaceutical company drug donations(Node #371075)
Donations by pharmaceutical companies of mectizan for river blindness, mebendazole to eliminate intestinal parasites, and azithromycin to treat trachoma have supported health agencies and benefited millions of persons with debilitating diseases – and illustrate who public-private partnerships can also promote health.
Self-regulation in the forestry and fisheries industries(Node #371074)
Corporate interests are often in tension with public health interest(Node #351052)
Self-regulatory measures often struggle to accomplish sufficient public health impact, as corporate financial interests are often in tension with the public health interest.
Public Health Responsibility Deal(Node #352457)The Public Health Responsibility Deal aims to tap into the potential for businesses and other influential organisations to make a significant contribution to improving public health by helping us to create this environment. The Responsibility Deal embodies the Government’s ambition for a more collaborative approach to tackling the challenges caused by our lifestyle choices.
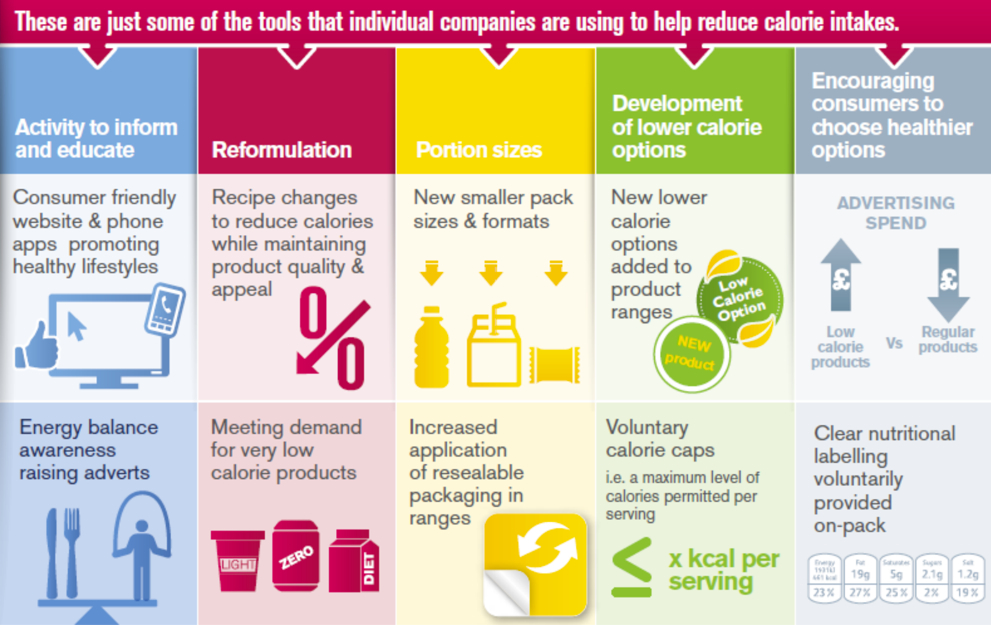
Examples of some of the approaches used by the food industry to reduce calories under the government’s Public Health Responsibility Deal Calorie Reduction Pledge.
Responsibility Deal
The government’s approach to working with industry is not to mandate action but to create voluntary agreements through the Responsibility Deal. The Public Health Responsibility Deal brings together the government, industry, the voluntary sector, non-governmental organisations and local government to voluntarily agree the actions they can take to help people make healthier choices. Organisations signing up to the Responsibility Deal commit to voluntarily improving public health through their responsibilities as employers, as well as through their commercial actions and their community activities and to reporting annually on the action they have taken in response to pledges they sign up to.
Collective pledges on alcohol, food, health at work and physical activity set out the specific actions that partners agree to take in support of the core commitments. The following collective pledges (with the most recent first) support the core commitment to encourage and enable people to adopt a healthier diet.
Pledges
• “Recognising that the Call to Action on Obesity in England set out the importance of action on obesity, and issued a challenge to the population to reduce its total calorie consumption by 5 billion calories (kcal) a day, we will support and enable our customers to eat and drink fewer calories through actions such as product/ menu reformulation, reviewing portion sizes, education and information, and actions to shift the marketing mix towards lower calorie options. We will monitor and report on our actions on an annual basis.”
• “We will provide calorie information for food and non-alcoholic drink for our customers in out of home settings from 1 September 2011 in accordance with the principles for calorie labelling agreed by the Responsibility Deal.”
• “We commit to the salt targets for the end of 2012 agreed by the Responsibility Deal, which collectively will deliver a further 15 per cent reduction on 2010 targets. For some products this will require acceptable technical solutions which we are working to achieve. These targets will give a total salt reduction of nearly 1g per person per day compared to 2007 levels in food. We recognise that achieving the public health goal of consuming no more than 6g of salt per person per day will necessitate action across the whole industry, Government, NGOs and individuals.”
• “We have already removed, or will remove, artificial trans-fats from our products by the end of 2011.”
The Department is currently developing a pledge on salt for catering, and fruit and vegetable consumption.
Annual feedback provided to the Department of Health shows Responsibility Deal partners are taking action on calories.
Big names such as Britvic, Burton’s Biscuits, Coca-Cola, Mars, Mondelēz, Nestlé, Premier Foods and Unilever, all of the major retailers as well as high street chains JD Wetherspoon and Subway included.
These are some of the actions already taken on reducing calories:
- Tesco: Reduced the number of calories sold in its own brand soft drinks by over 1 billion in 2012.
- Sainsbury’s: Reduced the sugar content of its own brand high juice squashes by between 4 and 10%, removing over 600 million calories from customers’ baskets per year; as well as removing 23 tonnes of saturated fat from the pastry in its biggest selling mince pies.
- Coca-Cola: Sprite now contains 30% fewer calories.
- JD Wetherspoon: Reduced the calories in 12 dishes.
- Nestlé: Over half (54%) of Nestlé confectionery now contain less than 110 calories per serving.
- Mars: On way to reducing the calories in all its chocolate products to no more than 250 calories per portion (by end 2013); with further reductions in some leading products, including Twix (from 284 to 248 calories). Has also launched the Maltesers Teasers chocolate bar (186 calories per bar).
- Burton’s Biscuits: Changes to the ingredients across all its brands will result in an estimated national reduction of 700,000 kcals per day for its customer in 2013.
- Subway: In 2012, Subway spent around 65% of its promotional budget on healthier eating; and launched a new range of low fat flatbreads.
- Morrisons: Launched a new healthier range, NuMe, which includes lower calorie options on an extended range of products.
- Aramark and Beefeater are now offering meals of less than 500 calories
- Britvic is to remove its full sugar Fuit Shoot from the market
Invest in weight management services(Node #352373)The departments of health in the four nations should extend and increase the provision of weight management services across the country, to mirror the provision of smoking cessation services.
Cost-effective interventions to reduce obesity in the UK
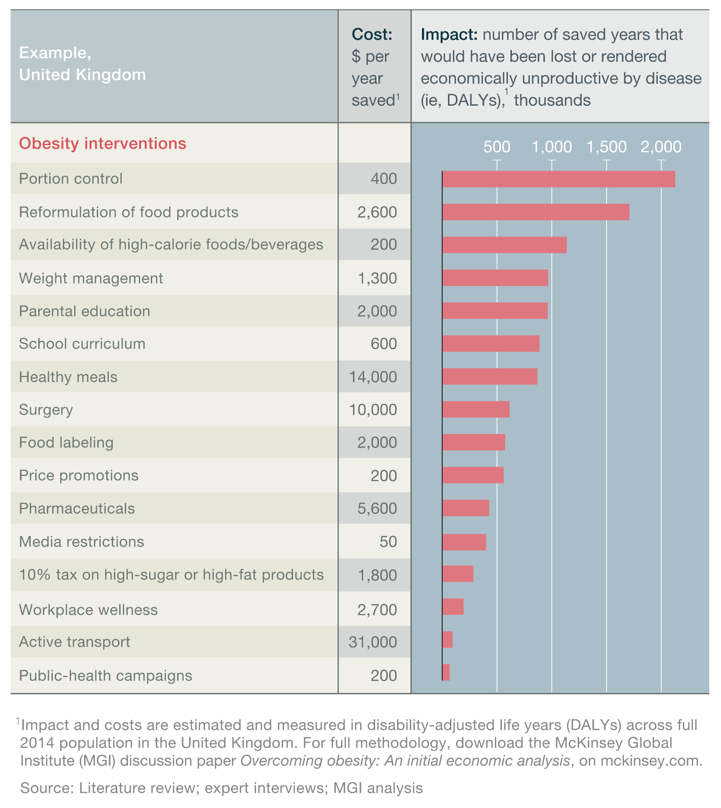
Offer financial weight loss incentives to people(Node #352847)
Offer financial weight loss incentives to people to become a healthier weight.
Providers should be formally evaluated and accredited(Node #370340)
Formal evaluation and accreditation introduces time delays(Node #370341)
Types of weight-management services(Node #366483)
Commercial weight-management programs(Node #366551)
Commercial provision of weight-management programs (e.g., Weight Watchers) that include group counseling, goal setting, and community support.
Health-system group counseling(Node #366549)
Health system provides a short-term (e.g., 12-week) group counseling program on nutrition and how to change dietary and physical activity behavior.
Health-system individual counseling(Node #366548)
Health system provides a short-term (e.g., 12-week) one-to-one counseling program on nutrition and how to change dietary and physical activity behavior.
Personal technology to support healthy eating and physical activity(Node #366547)
Personal technology to support healthy eating and physical activity: cross-platform –Health systems/employers provide personal technology platforms to support goal setting, tracking, and measuring of key behavior and health outcomes.
Physical activities on prescription(Node #366550)
Health system prescribes physical activities and provides free gym membership or other facilitative measures.
Short-term, intensive weight-management programs: adults(Node #366552)
Health-care system or commercial market provides short-term (e.g., two- to six-week) residential “boot camp” providing nutritional education and physical activity to adults.
Short-term, intensive weight-management programs: children(Node #366553)
Health-care system or commercial market provides short-term (e.g., two- to six-week) residential “boot camp” providing nutritional education and physical activity to children.
Weight management around childbirth (Node #366554)
Health-care system provides weight-management advice as part of pre- and postnatal care.
Early intervention programmes(Node #370332)
The investment in weight management services should include greater provision for early intervention programmes.
Improve support for people with severe and complicated obesity(Node #348686)
Greater focus needs to be devoted to strategies supporting individuals who are already obese. Current government policy is focused largely on prevention, which is vital in ensuring the scale of the obesity problem and its associated costs do not increase. It does not, however, address the problems of those people already obese or morbidly obese and the costs associated with their health conditions. Moreover, obesity treatment is often cost effective.
Develop a patient charter for those with obesity problems(Node #352569)
Multidisciplinary teams to cover severe and complex obesity across UK(Node #352562)Commissioning of specialist obesity services should be for multidisciplinary care of ‘severe and complex obesity’ and not directly for rather than just bariatric surgical treatment. Need multidisciplinary teams (MDTs) available to cover severe and complex obesity throughout the UK.
- In our hospitals there are few ‘joined up’ services for people who are overweight or obese; there is a need to develop and integrate weight management services with those healthcare services that manage the complications and conditions which arise from obesity such as coronary heart disease (CHD), diabetes, arthritis, sleep disorders and gynaecological disorders.
- Multidisciplinary teams have a proven track record in cancer care to promote quality by providing integrated services for patients, and we recommend that this model is translated to obesity.
1 All members of the multidisciplinary team (MDT) should be trained and experienced in motivational interviewing and incorporate these techniques into their clinical practice.
2 Since type 2 diabetes is common among the overweight and obese population, and management of obesity may directly affect diabetes prevention and management, integration with diabetes services is recommended.
3 Adoption of the Edmonton Obesity Staging System (EOSS) will allow better 'phenotyping' of the individual patient and facilitate audit and outcomes review and research.
4 The primary care team has an important role in signposting to relevant services which are known to be effective. Many patients may contemplate commercial programmes, or increasingly such services maybe providers of care within the NHS, and request advice from the primary care team. It is vital to ensure that patients attend services most suited to them.
5 The specialist MDT needs expertise in multiple obesity-related disorders. The MDT should include specialist consultant physicians, consultant surgeons, dietitians, nurses, psychologists and psychiatrists and exercise/physical activity professionals.
6 A particular issue amongst patients with extreme obesity is the increased prevalence of psychiatricdisorders, including eating disorders, anxiety and depression. Thus, close collaboration with primary care and mental health services is required to assist patients with significant psychological trauma or psychiatric illness.
7 A growing number of patients within primary care will have had bariatric surgery (sometimes performed outside the UK), and links with the (hospital-based) medico-surgical MDT are essential.8 Adequate administrative support to ensure that patients move smoothly through the MDT assessment is essential.
RCP oversee the development of multidisciplinary bariatric services(Node #352589)
The Royal College of Physicians (RCP) should oversee the development of multidisciplinary bariatric services to cover the population in the UK.
RCP should provide courses to train doctors in MDT formation(Node #352590)
The RCP should promote the provision of these multidisciplinary groups by developing and providing courses that advise, encourage and train doctors (and other healthcare professionals) on their formation.
Bariatric surgery can be cost effective(Node #352716)
Analysis by the Office of Health Economics estimated that between around 10,000 and 140,000 of patients could receive bariatric surgery based on the assumption of between 1% and 25% of patients eligible for surgery choosing to take this option. Overall the economic benefit ranged between £382m and £1,295m savings after three years to the NHS after surgery if 25% of patients potentially eligible for surgery chose this option.
Surgical management can be more costly than non-surgical management(Node #352715)
Surgical management was more costly than non-surgical management in each of the three patient populations analysed (BMI 40; BMI 30 and<40 with type 2 diabetes at baseline; and BMI 30 and <35) but gave improved outcomes. For morbid obesity, ICERs ranged between £2,000 and £4,000 per QALY gained. For BMI 30 and <40, ICERs were £18,930 at 2 years and £1,397 at 20 years, and for BMI 30 and <35, ICERs were £60,754 at 2 years and£12,763 at 20 years.
NICE guidance has been ignored on bariatric services(Node #370347)
An investigation by GP newspaper published in December 2014 found that over half of the UK's primary care organisations (PCOs) do not follow NICE or SIGN guidance on bariatric surgery [2].
Pharmacological treatment can be cost-effective(Node #352714)
A systematic review of pharmacological treatment in primary care (orlistat, sibutramine and rimonabant– the latter two now withdrawn) has shown all were effective at reducing weight and BMI, and cost effective when using a threshold of £20,000 per QALY.
Many smaller providers lack formal evidence to support interventions(Node #370339)
While some of the larger commercial providers have had their efficacy assessed by means of randomised control trials and other evaluative methods, many smaller providers have no such formal evidence to support their interventions.
Most obese UK children lack access to weight management programmes(Node #370331)
The majority of obese children in the UK don't have access to an evidence-based, proven, multicomponent child weight management programme as recommended by NICE (2006).
Weight management service provision is poor in comparison to smoking(Node #370334)
From a clinical perspective, weight management provision needs to mirror the coverage that smoking cessation services have achieved; yet, the investment in smoking cessation programmes remains significantly higher than the investment in weight management programmes. As a comparator, the NHS spent £88.2 million on smoking cessation services in 2011/12.
Weight management services are in short supply(Node #370330)
The Academy of Medical Royal Colleges notes that doctors don't have sufficient services available to refer people – that there are a limited number of well-designed fully evidence-based, effective and transferable weight management programmes, available for use in routine NHS primary care.
Weight management services can save more money than they cost(Node #370338)
Some well-designed fully evidence-based, effective and transferable weight management programmes are even economically ‘dominant’ (i.e. they save the NHS more money than it costs to provide the service).
Increase investment in obesity research(Node #352563)
Ensure that PSAs and LAAs fully reflect government obesity targets (Node #352781)
Ensure Public Service Agreements and Local Area Agreements fully reflect government obesity targets.
Public-health campaigns on obesity(Node #352728)Government launches comprehensive public-health campaigns promoting healthy habits across various media (e.g., TV, radio, out-of-home advertising). More impactful communication of the evidence base on obesity.
Cost-effective interventions to reduce obesity in the UK
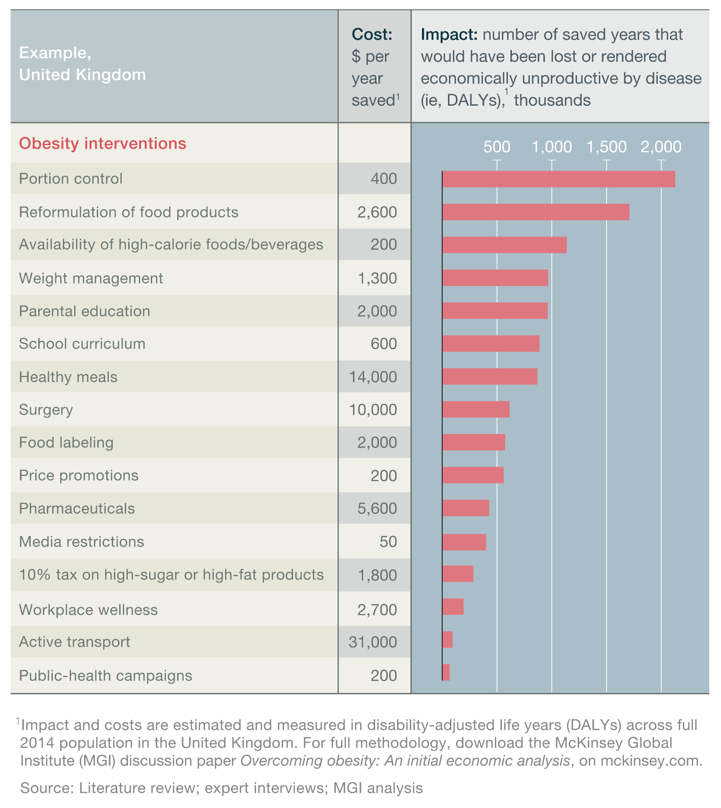
Spread social norms that support people to be health-desirable weight(Node #352844)
Encourage stronger personal will power(Node #348763)
Promote healthier social role models (Node #352837)
Positive messages focused on healthy behavioural changes work best(Node #386227)
A recent study [1] examining public perceptions of obesity-related public health media campaigns found that: people responded most favorably to messages involving themes of increased fruit and vegetable consumption and messages involving multiple health behaviors; messages with stigmatizing content produced the lowest intentions to comply; and messages that focused on making healthy behavioral changes without reference to body weight or obesity were perceived to be most positive and motivating.
Some degree of public regulation is necessary(Node #351051)
Some degree of public regulation is necessary to achieve public health targets on obesity – and this needs to be supported by standards set and monitored by public health expert committees to improve industry performance in the nutritional quality of food products and in marketing the products to children.
Invest in employee health and wellbeing(Node #352718)Encourage organisations to invest employee health and wellbeing; including a health risk assessment and the provision of resources to help employees address the factors that pose the greatest risk to their health and wellness. [1], [2], [3], [4], [5]
1. Employers should encourage healthy eating among staff by:
• implementing the National Institute for Health and Clinical Excellence (NICE) recommendations for obesity in the workplace (NICE CG43) [2]
• ensuring that healthy food is available in the workplace at affordable or subsidised prices
• encouraging nutritional labelling to allow employees to make informed food choices
• setting strict nutritional criteria as part of procurement contracts for food made available in food outlets and vending machines.
2. Employers should encourage physical activity by:
• signposting to and encouraging the use of walking and cycling routes and stairs, including the provision of safe cycle storage areas
• recommending the use of active travel methods to and from work, and provision of changing room facilities
• working with local authorities to enhance access to health services by public transport
• considering the use of staff incentives such as discounted membership of fitness clubs.
3. Employers should encourage healthy behaviour change by:
• developing a strategy for staff health and wellbeing
• encouraging staff to take regular breaks to move around as well as sufficient time to eat well
• using innovative ways to encourage lifestyle change amongst staff, e.g. intranet messages on health, and signposting local activity/weight management opportunities
• using staff training as an opportunity to ensure that leaders are aware of the importance of encouraging proactive approaches to staff health
• enabling equitable staff access to a range of weight management and activity options, by commissioning weight management services which have proven effectiveness.
4. Occupational health departments have a responsibility to diagnose overweight and obesity in new employees, and wherever employees make health contacts (eg winter influenza vaccination) to communicate the health benefits of weight loss, and signpost obese employees either to ‘in-house’ or community-based services. Occupational health services could contribute to the monitoring of those engaged in weight management programmes by providing weighing facilities and information on healthy eating and activity opportunities within and outside the workplace.
Cost-effective interventions to reduce obesity in the UK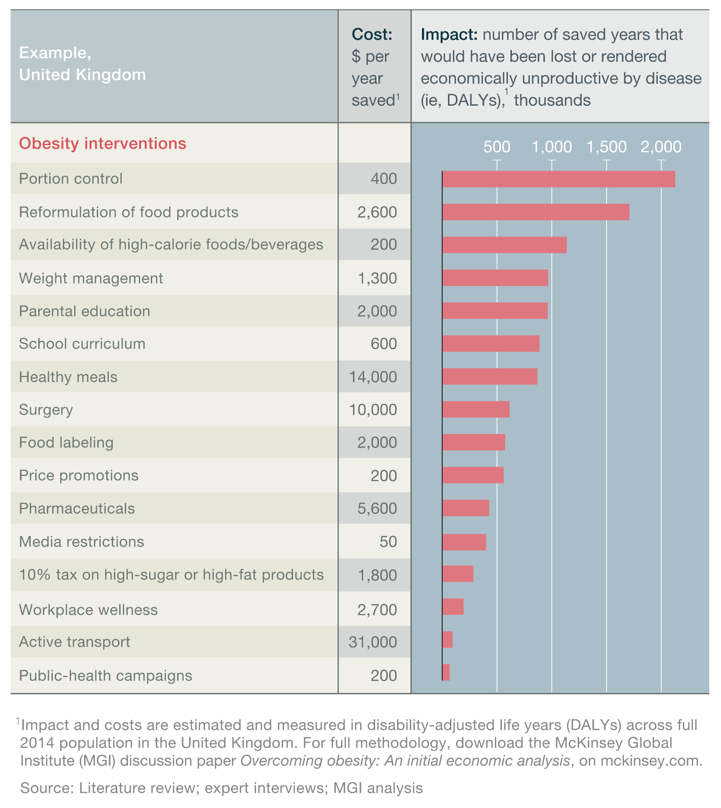
Active self-regulation and KPIs that work for health (Node #352834)Active self-regulation and Key Performance Indicators that work for health.
8 Risks and Behaviors drive 15 Chronic Conditions that account for 80% of total costs for all chronic illnesses worldwide.
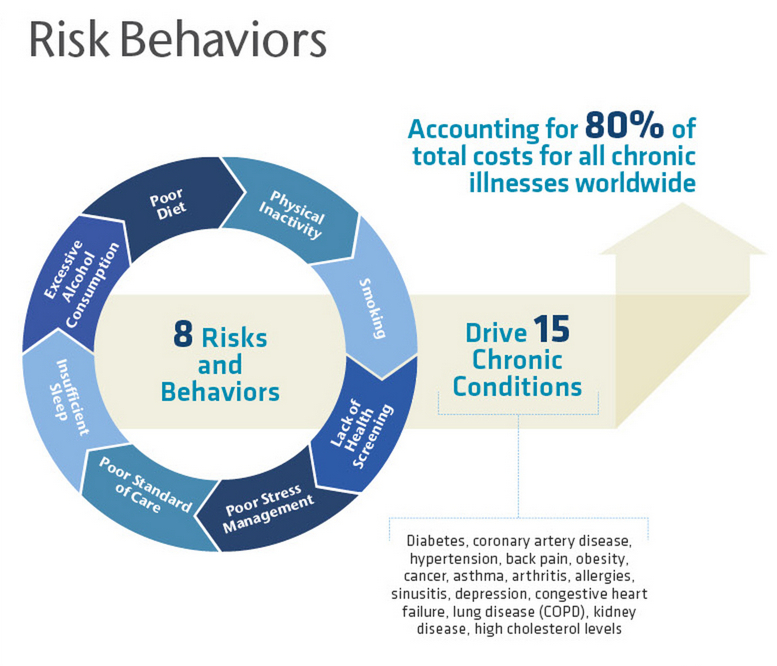
Break a workforce into three categories. There's the healthy part of the population, those who are at risk, and the third part, which we call 'in the system' [people being treated for chronic conditions]. You want to design strategies not only about wellness, but overall plan creation and communications strategies that are a dimensional integration between your population's health, the demographics of that population and the three segments—the healthy, the 'at risk' and those who are in the system.
Ensuring health targets are built into wastage reduction targets (Node #352823)
Better weight management resources for obese healthcare workers(Node #352565)Better weight management resources for healthcare workers who have an obesity problem.
"In many ways, today’s workplaces promote—or at least enable—poor eating habits and physical inactivity, says Arla Day, PhD, Canada Research Chair, Industrial and Organizational Psychology, at Saint Mary’s University in Halifax.
'A lot of workplaces offer no access to healthy eating options,” she says. In addition, many jobs involve sitting at a desk in front of a computer all day.'
And if you are sedentary for eight hours, that’s both strike one and two against you,” she adds, noting that some experts think that sitting is the “new smoking” in terms of impact on health. Strike three is experiencing high workplace stress and being treated poorly at work. Stress can be particularly detrimental in maintaining or managing your weight. Not only are the biological effects of chronic stress directly related to the development of obesity, but unhealthy coping mechanisms, such as overeating and physical inactivity, may also contribute to weight gain.
'When people are under stress, their eating can become disordered—skipping meals, binge eating—which can lead to obesity, and which then can lead to more stress, so that it can continue as a downward cycle,' says Dr. Day." [2]
Employers give employees financial incentives to improve health(Node #366557)
Employers provide material incentives to individuals for improved key health indicators (e.g., discounts on insurance premiums, gym membership, prizes).
Collaboration between workers and management in the program design(Node #373485)
Coercive financial incentives produce short-lived results at best(Node #392284)
Scant evidence on the effectiveness of wellness financial incentives(Node #373483)
"Although it may seem obvious that charging higher premiums for smoking (or high body mass index, cholesterol, or blood pressure) would encourage people to modify their habits to lower their premiums, evidence that differential premiums change health-related behavior is scant. Indeed, we’re unaware of any insurance data that have convincingly demonstrated such effects."
Discovery Health's Vitality Programme(Node #373020)Discovery Health, South Africa's largest private health insurer with over 2.5 million beneficiaries, developed a successful incentivized health promotion programme called "Vitality", which includes health risk assessments, subsidized gym memberships and smoking cessation or weight loss programmes with many incentives (including cash back on purchases of healthy foods).
PruHealth Vitality – UK(Node #373023)"Vitality is health and life insurance that rewards you for being healthy. It’s the nudge to get you off the sofa, it’s the motivating friend with helpful tips to improve your life, and it’s a proven way to get healthier and be rewarded."
Safeway Health(Node #373482)Safeway is delivering a holistic approach to health, wellness and fitness to its employees and their families with initiatives that improve their health and motivate them to become accountable, quality- and cost-conscious health care consumers.
Safeway's costs began to flatten three years before 2008 program began(Node #373484)
Safeway's health program began in 2008 too late to deserve credit for flat costs starting in 2005.
Employers offer team challenge incentive schemes in the workplace(Node #366555)
Employers provide team challenge activities to encourage physical activity and improved key health indicators in the workplace.
Reverse the long working-hours culture(Node #352846)
Strong business case for investment in employee health and wellbeing(Node #371613)
Investing in the health and wellbeing of employees makes business sense. It has been estimated that working age ill-health costs the UK £100 billion per annum, more than the annual budget for the NHS. In 2009–10, 23.4 million days were lost due to work-related ill-health.
Reduce incidence of workplace injuries(Node #392571)
Excess weight also significantly increases the risk of workplace injuries (e.g. back injuries and falls); some evidence suggests that individuals are 40% to 50% more likely to experience a gamut of injuries at work if they fall in the overweight category. [1]
Reduce the costs of absenteeism(Node #352751)
Reduce the costs arising from employee’s intentional or habitual absence from work.
Reduce the costs of presenteeism(Node #352752)
Presenteeism is defined as “the problem of workers being on the job, but, because of illness or other medical conditions, not fully functioning”.
Japan's Metabo Law(Node #379162)Japan introduced a set of guidelines – the Standards Concerning Implementation of Special Health Examinations and Special Public Health Guidance under the Ministry of Health, Welfare, and Labor Order 159 (the "Metabo Law") – on April 1, 2008 to address national concern that half of all men and 1 in 5 women between the ages of 40 and 74 were showing signs of metabolic syndrome.
Manansala notes [1] that the guidelines:
- aimed to reduce the overweight population by 10% over the 5 years and by 25% over the next 7 years.
- called for local governments and employers to conduct mandatory annual examinations, including measurement of waistlines for people between the ages of 40 and 74 (44% of the population). [3]
- required individuals who exceeded the maximum waist line of 33.5 in (85 cm) for men and 35.4 in (90 cm) for women, and who doctors determined were in the most severe category, to attend counseling sessions over the next three months to lose weight and make lifestyle changes. [2]
- required employers to ensure a minimum of 65% participation with the exam and 25% reduction in obesity within 7 years (or face penalties of up to 10% of the current payments – which would go to fund elderly care.
Encouraged companies to offer employees healthier food choices(Node #379166)
Encouraged firms to offer health education to employees and families(Node #379167)
Fines from the 2015 deadline will fund healthcare for the elderly(Node #379165)
Increased awareness of health and fitness in Japan(Node #379163)
Japan remains one of the thinnest countries in the world(Node #379164)
Less than 50% of people are attending the required annual check-ups(Node #379168)
Only 12.3% of people receiving counseling act on medical advice(Node #379169)
Risk that companies will discriminate against overweight people(Node #379170)
Companies may start to discriminate against overweight people to avoid paying the fines (which, in a large company like NEC, could amount to $19m).
The Metabo Law does not address rising childhood obesity rates(Node #379171)
The waist-line measurement conflict with the IDF recommendations(Node #379172)
The waist-line measurement conflict with the International Diabetes Federation recommendations.
Who should invest in employee health and wellbeing?(Node #400393)
Improve the costs and outcomes of medical interventions(Node #366812)
Incentivise GPs to improve patient outcomes(Node #348678)The Quality and Outcomes Framework should be amended to provide incentives for GPs to proactively offer advice to overweight and obese patients and refer them to weight management services where appropriate, rather than simply keeping a register of these patients. [1]
- As things stand, the Quality Outcomes Framework simply requires GPs to register obese patients and effectively penalises GP for taking action to improve their patients’ outcomes and help remove them from the obesity register. GPs should be encouraged to engage with patients on obesity and weight management issues.
Focus outcomes indicators on action by primary health professionals(Node #348679)The Quality Outcomes Framework indicators on obesity should include, and focus on, indicators on the action taken by primary healthcare professionals on behalf of overweight or obese patients. [1]
- The QOF should contain an indicator that would award points to incentivise and encourage GPs for providing advice on weight management and recommending appropriate guidance and support from the wide range of resources available to tackle obesity, including the range of structured community based weight management programmes which are available.
The Quality and Outcomes Framework(Node #348695)The QOF was introduced in 2004 as a voluntary incentive scheme for GP practices in the UK. It contains groups of indicators against which practices score points according to their level of achievement, with a higher score leading to higher financial rewards. The aim of the QOF is to highlight priorities for improving patient care and provide incentives for GPs to drive up quality in these areas.
- QOF indicators are intended to identify areas where responsibility lies mainly with GPs in primary care, where there is evidence of health benefits from improved primary care, and where the disease is a priority in a number of the devolved nations.
- One QOF indicator relates to obesity:
“if a practice can produce a register of patients aged 16 or over and with a BMI greater than 30 in the preceding 15 months” then eight points are added to the QOF score.
- However, this indicator requires no action – aside from the production of a register – to be taken for any points to be received.
- GPs should be provided with better incentives to tackle obesity before it leads to major health complications.
Improve surgical interventions for obesity(Node #366481)The Cochrane Review [1] concluded:
- Surgery results in greater improvement in weight loss outcomes and weight associated comorbidities compared with non-surgical interventions, regardless of the type of procedures used.
- When compared with each other, certain procedures resulted in greater weight loss and improvements in comorbidities than others. Outcomes were similar between RYGB and sleeve gastrectomy, and both of these procedures had better outcomes than adjustable gastric banding. For people with very high BMI, biliopancreatic diversion with duodenal switch resulted in greater weight loss than RYGB. Duodenojejunal bypass with sleeve gastrectomy and laparoscopic RYGB had similar outcomes, however this is based on one small trial. Isolated sleeve gastrectomy led to better weight-loss outcomes than adjustable gastric banding after three years follow-up. This was based on one trial only. Weight-related outcomes were similar between laparoscopic gastric imbrication and laparoscopic sleeve gastrectomy in one trial.
- Across all studies adverse event rates and reoperation rates were generally poorly reported. Most trials followed participants for only one or two years, therefore the long-term effects of surgery remain unclear.
Cost-effective interventions to reduce obesity in the UK
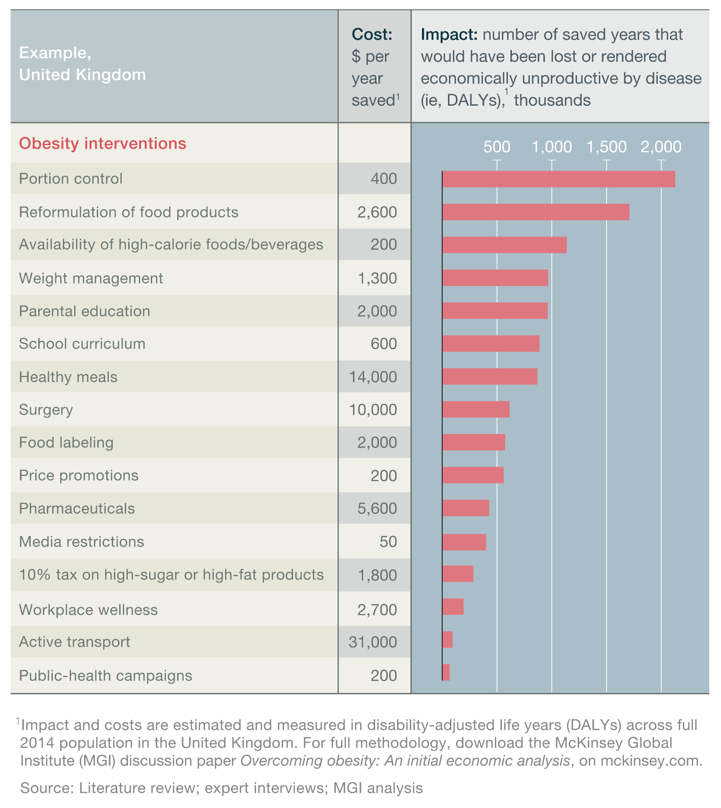
Bariatric surgery: gastric banding(Node #366542)
Provision of gastric-banding surgery
Bariatric surgery: gastric bypass(Node #366543)
Provision of gastric-bypass surgery.
Set up a specialist group of bariatric nurses(Node #352566)
The Royal College of Physicians in conjunction with the Royal College of Nursing should up a specialist group of bariatric nurses who are trained in the specialist aspects of bariatric medicine and surgery, including post-surgery follow-up.
Surgical and pharmaceutical solutions don't resolve societal problems(Node #366897)
There is a danger of searching for pharmaceutical or bariatric solutions; as technological solutions are unlikely to resolve societal problems – at best, they are a ‘sticking plaster’.
Develop better pharmaceutical obesity therapies(Node #352710)Obesity drug sales are forecast to $3.8bn globally in 2018 [2]—in comparison to $57bn for Diabetes drug sales[2]—with evidence suggesting that the modest average weight losses achieved with current anti-obesity agents may be of some clinical benefit [5]. However, the current generation of drugs, which act on the central nervous system to suppress appetite, have raised significant health concerns—including psychiatric disorders, such as suicidal behaviour, depression, and cardiovascular problems.
Cost-effective interventions to reduce obesity in the UK
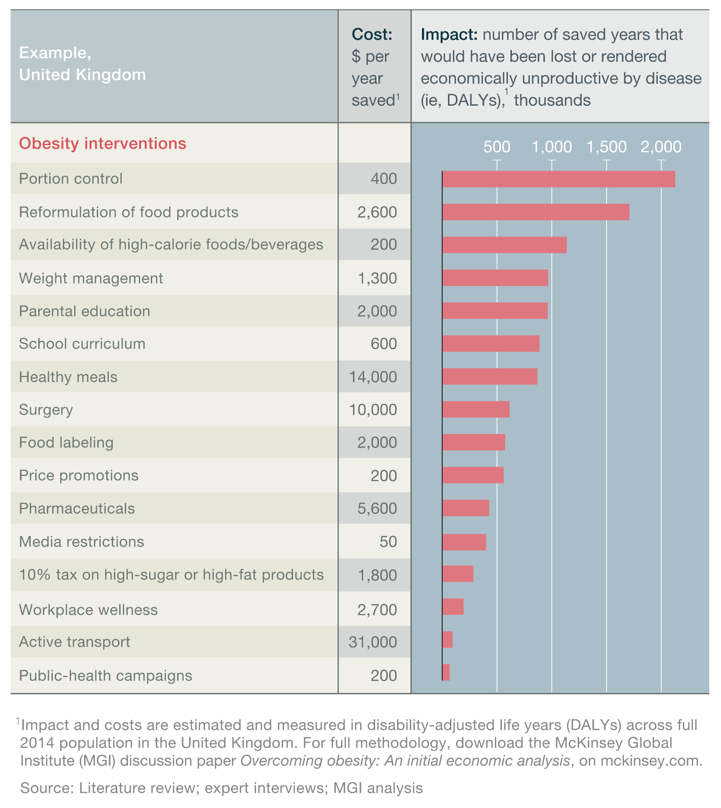
Over-the-counter pharmaceuticals(Node #366521)
Provision of non-prescription weight-loss drugs.
Prescription pharmaceuticals(Node #366522)
Medical prescription of weight-loss drugs.
Develop new technologies to support healthier behaviour(Node #352711)
Develop innovative technologies and applications to support healthier life choices including more physical activity and healthier diets.
Mobile health and weight-loss applications(Node #372853)
Around 2,000 weight-loss apps are currently available on the iPhone, and 500 million people were expected to be using mobile health applications by 2015. [1]
Fecal microbiome therapy(Node #392581)
Modification of gut microbiota appears to be a promising therapeutic intervention for obesity and other metabolic disorders. [1], [2]
Undertake a systematic review of specialist obesity services(Node #352570)
Undertake a systematic review of specialist obesity services between the Royal College of General Practitioners community leads and the Royal College of Physicians (RCP) and learned societies, including the Society for Endocrinology, Diabetes UK and the Association of British Clinical Diabetologists
Many obesity policy measures appear to be cost-effective for society(Node #371556)The recent MGI study [1] reported that almost all of the obesity policy interventions included in its economic analysis appeared to be highly cost-effective at the societal level—i.e. the health-care costs and productivity savings that accrue from reducing obesity through a specific intervention outweighed the direct investment required to deliver that intervention when assessed over the full lifetime of the target population.
Cost-effective interventions to reduce obesity in the UK
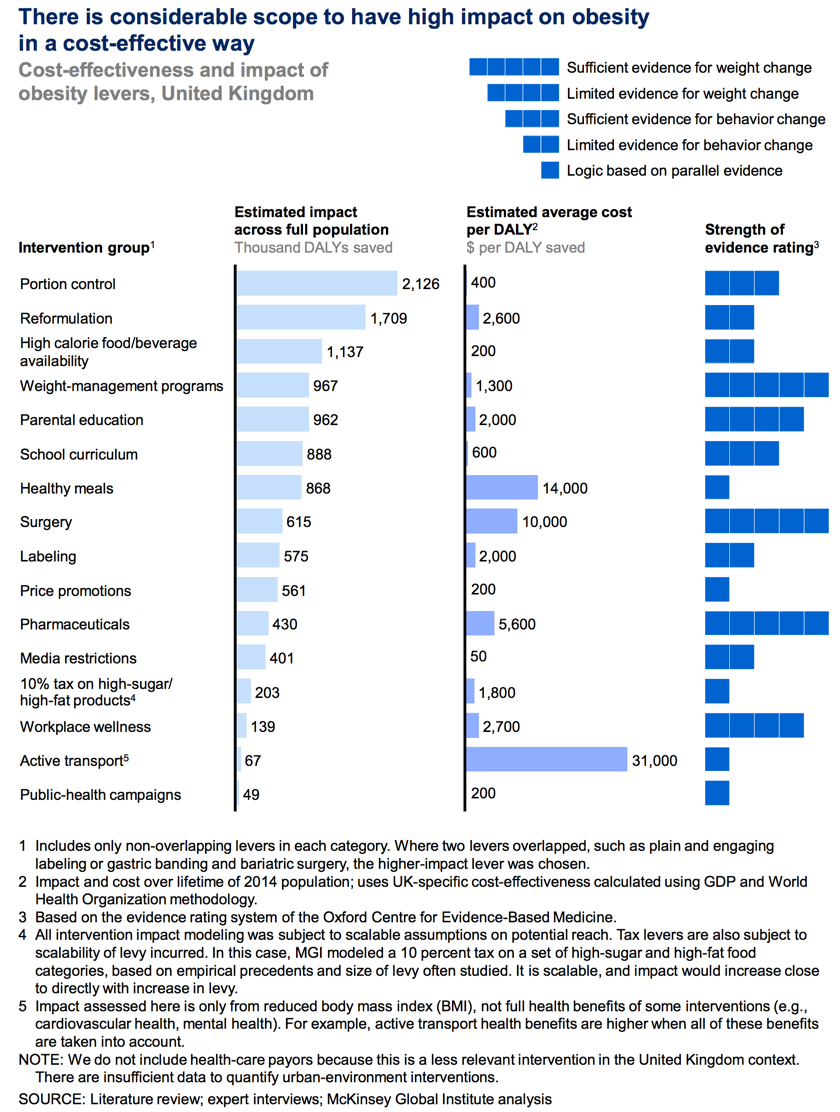
Birmingham's Be Active Programme(Node #374635)Birmingham's Be Active Programme returned on average £21.3, and up to £23 in benefits for every £1 spent in terms of improved quality of life, reduced NHS use, productivity and other gains to the local authority.
Glasgow Health Walks(Node #374634)In 2011–12 the Glasgow Health Walks project led to a return on investment of £8 for every £1 spent.
Scarce health resources would be better spent elsewhere(Node #371555)
Framing obesity as a health crisis results in scarce health resources being directed to millions of people who are already healthy.
Barriers to change(Node #352796)
What are the barriers to tackling obesity?
Policy process struggles to address multi-factor, systemic problems(Node #366900)
Definitive evidence is often difficult to obtain(Node #352797)
"When dealing with complex systems it is rarely possible to obtain the sort of evidence that would be required in science, engineering or clinical trials. As things stand, the overall evidence base on how to tackle obesity is limited, and what evidence there is on effective approaches is skewed towards short ‘visible’ interventions at an individual and consumer level." [1]
Need to appreciate and incorporate multiple perspectives(Node #352799)A second dimension of complexity requires an appreciation of the different perspectives used by agents and agencies within the system (pluralism). Most of the population, including many experts and scientists, are not able to dis-identify from their own perspective sufficiently to be able to appreciate other people's perspectives fully. Until all the key perspectives are incorporated into a study then any analysis will be partial and any intervention likely to fail. [1]
"Within complex systems it is normal for there to exist radically different perspectives about how the system works or ought to work. The existence of these different perspectives adds significantly to the complexity of the system‟s operation, in part because messages and data will be interpreted differently by people with different perspectives and also because different agents and agencies are likely to be pursuing competing goals." [1]
Relational complexity of problems makes them hard to grasp as a whole(Node #352798)
Obesity is a complex, systemic issue with no single or simple solution. Within complex systems it is normal for there to exist a complex network of causes that frequently feeds back on itself. The systems that have been modelled mathematically indicate that the overall behaviour of the system is determined by the structure of these interactions (in particular feedback loops and delays) rather than the values of any particular variables or parameters. [1]
Short-term pressures and incentives undermine long term plans(Node #352805)
Desire for solutions undervalues real improvements(Node #352800)When dealing with complex human systems it is necessary to focus on improvements, not solutions. Sustainable change takes place slowly and as the result of co-operative action by large numbers of agents and agencies within the system. [1]
"The shift away from "solutions‟ toward "improvements‟ is also consistent with a recognition that it is impossible to have sufficient understanding or control of the context to predict the outcome of interventions in complex systems. It is therefore more realistic to aim for small improvements and to support this with a learning approach involving as many of the key agents and agencies in the system as possible. This approach also recognises that sustainable change in complex systems occurs slowly and requires continued attention to improving rather than a strategy or policy designed to „solve‟ the problem once and for all.
Another aspect of adopting a systems approach to issues is that it requires those involved to reflect on their own perspective and the implicit assumptions involved The challenge of exploring different framing of the issue is similar to, but not identical to, that of appreciating the perspectives of other agents or agencies within the system." [1]
Hard to initiate, resource, and sustain cross-boundary action(Node #352803)
Desire to prioritise options becomes a barrier to action(Node #366460)
A search for the “best” interventions or a single solution could delay action and displace responsibility. Given the seriousness of the obesity issue, the aim should be to do as much as possible as soon as possible. [1]
Government obesity efforts are too fragmented to be effective(Node #366457)
Government efforts to tackle the obesity issue seem too fragmented to be effective. In the United Kingdom, 15 central government departments; all local authorities with responsibility for health, education, and local planning; 16 EU directorates-general; and a wide range of nongovernmental organizations all have a significant impact on the major intervention areas. [1]
Polarization and obfuscation are used as tactics in resisting change(Node #366903)
Disproportionate financial power and resources of the industrial lobby(Node #352804)
Institutional inertia(Node #352802)In most human activity systems a change in the functioning of the whole system requires a significant number of people within the system to change; they may have to change some or all of their habits, behaviour and values. [1]
"When progress on an issue requires people to change their beliefs, behaviours or values then, according to Heifetz and co-workers, the issue is an "adaptive issue" and requires a different leadership style – known as Adaptive Leadership. [2]
One of the key insights from Heifetz‟s work is that people resist change because they perceive the losses more clearly than the benefits. The losses may be of familiarity, of dearly held values or beliefs, of some aspect of self-esteem or simply loss of resources or power.
Heifetz and his colleagues stress that one of the key tasks in facilitating change is to acknowledge these losses. What they do not emphasise is the degree to which this requires those fostering the change to appreciate the perspectives of those involved so that the nature and depth of loss can be acknowledged." [1]
Personal resistance to change(Node #352925)
Cognitive bias(Node #352926)
Cognitive biases are patterns of deviation in judgment, in which inferences about other people and situations are drawn in an illogical fashion.[1]
Availability heuristic(Node #352929)
People tend to overweight data that comes easily to mind, which is to say vivid (extreme) and recent examples.
Bandwagon effect(Node #352928)
People tend to believe that something is a better idea if a lot of other people are doing it.
Beneffectance(Node #352930)
People tend to view success as a result of their own actions, while they view failures as having been due to factors largely outside of their control.
Confirmation bias(Node #352931)
The tendency to look for data that confirms your theory, rather than data that falsifies it.
Hyperbolic discounting(Node #352932)
People value small short-term payoffs more than much higher long-term payoffs.
Information cascade(Node #352935)
An information cascade occurs where people dismiss their individual instincts and personal data and base their decisions on the choices made by previous decision makers—and their decisions in turn influence every subsequent person to do the same.
Optimistic bias(Node #352933)
People tend to be overconfident about their own abilities and the outcome of their plans.
Overconfidence bias(Node #352934)
People are too confident in the accuracy of their predictions.
Promotion of people with short-term, action bias(Node #352936)
People promoted to run top companies are typically selected for the ability to deliver immediate targets; this focus often makes them poorly equipped to take the more distanced, historical perspective necessary to spot the long-term trouble brewing.
Recency effect(Node #352927)
People tend to overweight recent events in considering the probability of future events.
Crisis fatigue and despondency about the potential for change(Node #372886)
With so many issues competing for public attention and resources, the stakeholders associated with each issue can feel systemic pressure to present the impact of their issues, and the urgency of the action required, in as dramatic a way as possible; a tendency that tends to be amplified by the commercial media's attraction to simple and dramatic headlines. This pattern can encourage public fatigue towards the language of crisis and a sense of despondency about the prospects for systemic change.
Current incentives are mis-aligned(Node #366458)
Debate on obesity is polarized and antagonistic(Node #366451)
Much of the global debate on obesity has become polarized and sometimes deeply antagonistic.
Epigenetic transmission(Node #370418)
Epigenetic dynamics suggests that a poor diet and lack of physical activity during pregnancy may result in a mother's child and grandchildren being more predisposed to obesity, diabetes and premature death (highlighting the potential intergenerational impacts and time delays arising from the current crisis).
Obesogenic environment damps impact of individual changes(Node #366666)
UK Health system is under severe pressure on multiple fronts(Node #370389)
The future health of millions of children, the sustainability of the NHS, and the economic prosperity of Britain all now depend on a radical upgrade in prevention and public health. Twelve years ago Derek Wanless’ health review [2] warned that unless the country took prevention seriously we would be faced with a sharply rising burden of avoidable illness. That warning has not been heeded – and the NHS is on the hook for the consequences. [1]
About this map(Node #371370)Our shared goal is to create a comprehensive and coherent visual representation of the obesity policy space—including the causes, impacts, policy actors, proposed interventions, evidence, guidance, and barriers to change—that can help us explore and understand the space as a systemic whole; that can be collaboratively and iteratively edited, refined, and evaluated by the policy community; and that provides a dynamic, open substrate for dialogue, learning and action across the policy community.
The Current Structure of the Maps
The current work-in-progress is presented as a cluster of three interlinked maps: (1) The main obesity policy discussion map, (2) the map of the obesity policy stakeholders, and (3) the map of the Foresight systems model:
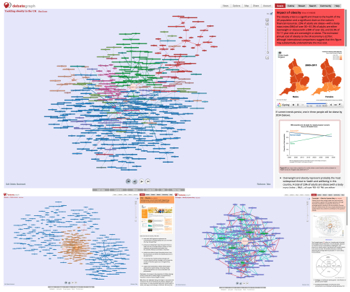
Although the scale of the mapping can seem overwhelming at first—particularly if you are new to DebateGraph—DebateGraph gives us a way to explore and deepen our understanding of the policy space through small manageable steps.
This process isn't effortless—it involves learning how to use DebateGraph and taking the time explore the maps—but it delivers high rewards:
(1) Exploring the map is a highly efficient way of deepening your understanding: the mapping team has spent hundreds of hours mapping and inter-linking a vast body of evidence and reports to develop insights that you can grasp in a few hours of exploration.
(2) The complexity of the obesity challenge is not infinite; just of a sufficient degree that it's difficult for us to hold and process it as a whole in our minds: DebateGraph helps us overcome this cognitive limitation by allowing us to externalise and work through this structure from our own starting point at our own pace.
(3) Moreover, this externalised structure isn't just the parts that are in our heads, it interweaves the disparate parts that are in many heads and allows us to see them as a coherent whole.
(4) The maps are living structures that continue to evolve and reshape as more people share their knowledge and insights and as more evidence emerges, and, once you have a feel for the structure of the map, it becomes almost effortless to keep with this process and to recognise the contextual significance of new information.
DebateGraph is also fun to play with, but it's not a toy: it has been designed by policy makers for policy makers to enhance our understanding systemic and network governance – and it has been used by the UK Prime Minister's Office, the White House Office of Science and Technology Policy, and the European Commission.
Exploring the maps
The Views menu (above) lets you toggle between different visualizations of the map or parts of the map – with each type of view having specific strengths and uses. You can also vary the behavior of each View type using the Options menu.
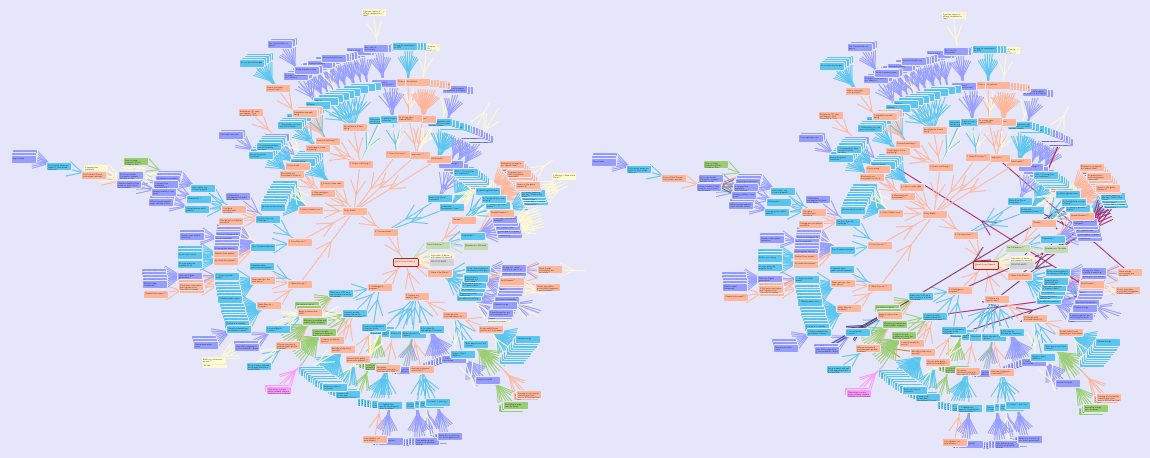
Contributing to the Map
There are various ways in which you can contribute to the development of the current map:
(1) Add a Comment to an idea, by clicking on the Comment button under the map. The process is just the same as commenting on a blog. Your comment will also appear in the Map activity stream and in the email digests to the Map community.
(2) Add a Citation to an idea, using either the Cite button (beneath the map) or the Cite radio button underneath the Details text. Citations are one of the easiest and most useful contributions you can make to a map; as they tell the map community about articles elsewhere on the web that you think are relevant to a particular idea and/or that contain ideas that you think should be added to the map.
(3) Add a new idea to the map by navigating to the relevant part of the map and then clicking on the Add idea button (beneath the map in the Hub view). Prior to adding a new idea, it's generally worth exploring the map and using the Search this map facility on the Finder tab to check whether the idea is included elsewhere on the map already. When adding a new idea, it's always fine to use the default Issue idea type (although you are also welcome to change the idea type using the color selector beneath the idea text entry box – and the idea selector will always guide you as to the types of idea that are available in any given location).
(4) Rate an idea, either by clicking on the Rating scale shown at the bottom of the Details text or by clicking on the arrow that points from the idea to its parent (which opens a small version of the rating scale on the map). Rating ideas in this way helps the community to see which ideas are perceived to be the most important (and why).
(5) You can also Edit an existing idea – for example, to correct a typo, to clarify or improve the text, to change the idea type, or to add more details to the Details text – either by clicking on the small Edit link (bottom left on the map in the Hub view) or by clicking on the Edit details link (at the bottom of the Details text). Each idea has a full Edit history; so you can always revert to an earlier version of the idea at any time.
...and each of these ways of contributing to a map is explained in more detail in its own section of the
Help tab.
Participating in the obesity map(Node #400383)The obesity mapping community is open for all to join and share their insights, experiences, stories, ideas and expertise – and after registering (via the Account menu above) you are welcome to start contributing to the community's learning straightaway.
Adding your insights to the map
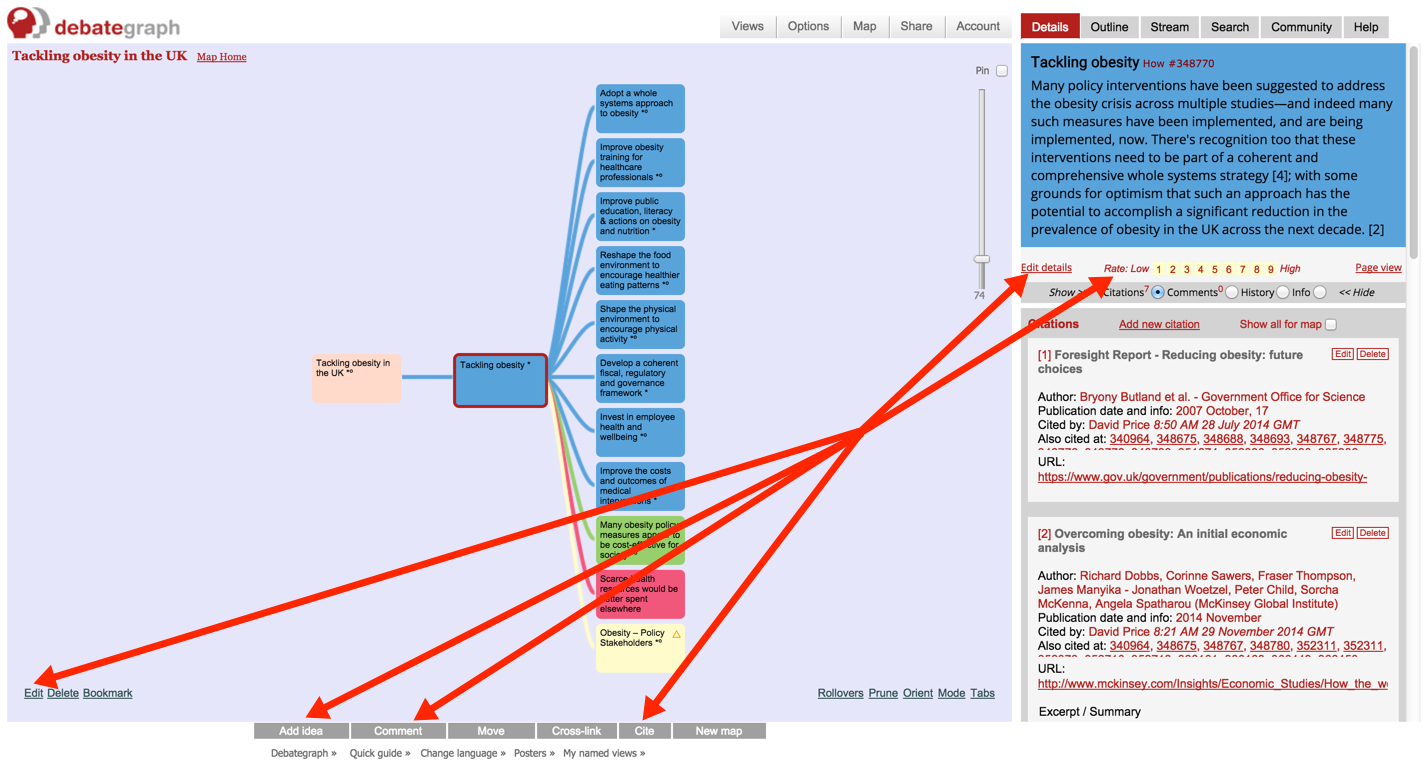
(1)
Add a Comment to an idea by clicking on the
Comment button beneath the map. Comments (which can include links) allow conversations to build about specific ideas (or the map as a whole) and are a quick and simple way to offer feedback and suggestions for further improvement.
(2)
Rate an idea by clicking on the
Rating scale shown at the bottom of the
Details text (on the right). Rating ideas helps everyone to see which ideas are perceived to be the most important by the community (and why).
(3)
Add a Citation to an idea using the
Cite button beneath the map. Citations are references to articles or papers that are relevant to a particular idea (and/or to the subject of the map as a whole).
(4)
Add a new idea to the map using the
Add idea button beneath the map – which adds and connects your new idea to the idea currently selected on the map. When adding a new idea, it's always fine to use the default
Issue idea type (which can be changed later at any time).
(5)
Edit an existing idea using the
Edit link (bottom left on the map) or the
Edit details link (at the bottom left of the Details text area, on the right of the screen). Each idea has a full
Edit history; so you can always revert to an earlier version of the idea at any time.
...and each of these ways of contributing to a map is explained in more detail in its own section of the Help tab.