|
![]()
| Invest in weight management services How1 #352373 The departments of health in the four nations should extend and increase the provision of weight management services across the country, to mirror the provision of smoking cessation services. | Cost-effective interventions to reduce obesity in the UK 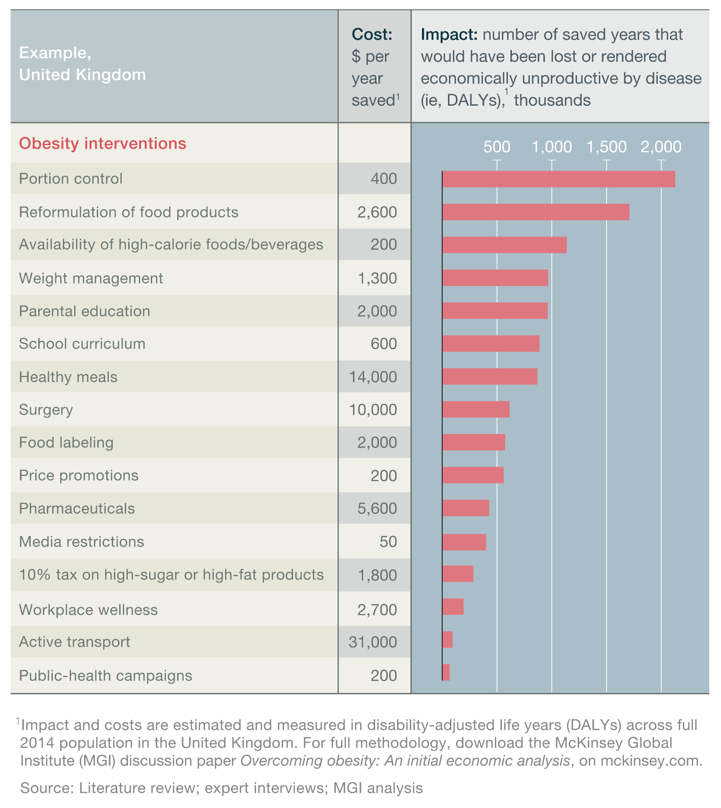
|
+Citavimą (2) - CitavimąPridėti citatąList by: CiterankMapLink[1] Measuring Up: The Medical Profession's Prescription for the Nation's Obesity Crisis
Cituoja: Academy of Medical Royal Colleges
Publication info: 2013 February
Cituojamas: David Price 8:03 PM 16 December 2014 GMT
Citerank: (67) 340964Tackling obesity in the UKWith concern growing that the Foresight analysis—that 50% of the UK population could be obese by 2050, at an annual cost to the nation of around £50 billion per year [2]—substantially underestimates the scale of the unfolding obesity crisis, the College of Contemporary Health is working with the wider policy community to develop a whole systems map of the obesity crisis and the potential responses.7F1CEB7, 348679Focus outcomes indicators on action by primary health professionalsThe Quality Outcomes Framework indicators on obesity should include, and focus on, indicators on the action taken by primary healthcare professionals on behalf of overweight or obese patients. [1]565CA4D9, 348700Health Professionals84E4A378, 348703Actions – Industry2794CAE1, 349151AMRCThe Academy of Medical Royal Colleges comprises the 20 medical Royal Colleges and Faculties across the UK and Ireland whose presidents meet regularly to agree direction in common healthcare matters. It provides a collective, clear and sure voice for the bene?t of patients and healthcare professionals across the four nations of the UK.58D3ABAB, 352368AMRC – RecommendationsThe AMRC presents 10 key recommendations – an ‘action plan’ – of steps that it believes must be taken to make real inroads into tackling the obesity crisis in the UK. The recommendations fall into three areas: actions to be taken by the healthcare professions; changing the ‘obesogenic’ environment; and making the healthy choice the easy choice.565CA4D9, 352369Actions to be taken by the healthcare professionsActions to be taken by the healthcare professions suggested by the AMRC.565CA4D9, 352370Changing the ‘obesogenic’ environment565CA4D9, 352371Making the healthy choice the easy choice565CA4D9, 352374Improve nutritional standards for food in hospitalsIntroduce food-based standards—in line with those put in place for schools in England in 2006—in all UK hospitals in the next 18 months; with commissioners working with a delivery agent similar to the Children’s Food Trust to put these measures into place.565CA4D9, 352375Increase support for new parentsThe current expansion of the health visitor workforce in England should be accompanied by 'skilling up' the wider early years workforce to deliver basic food preparation skills to new mothers and fathers, and to guide appropriate food choices which will ensure nutritionally balanced meals, encourage breastfeeding and use existing guidance in the Personal Child Health Record as a tool to support this.565CA4D9, 352376Improve nutritional standards in schoolsThe existing mandatory food- and nutrient-based standards in England should be applied to all schools including free schools and academies. This should be accompanied by a new statutory requirement on all schools to provide food skills, including cooking, and growing – alongside a sound theoretical understanding of the long-term effects of food on health and the environment.565CA4D9, 352377Reduce fast food outlets near schoolsPublic Health England should, in its first 18 months of operation, undertake an audit of local authority licensing and catering arrangements with the intention of developing formal recommendations on reducing the proximity of fast food outlets to schools, colleges, leisure centres and other places where children gather.565CA4D9, 352378Restrict junk food advertisingBan television advertisements of foods high in saturated fats, sugar and salt before 9pm, and seek agreement with commercial broadcasters not to advertise these foods on internet ‘on-demand’ services. [2]565CA4D9, 352379Pilot a 20%+ tax on all sugary, soft drinks for 1 yearFor an initial one year, a duty should be piloted on all sugary soft drinks, increasing the price by at least 20%. This would be an experimental measure, looking at price elasticity, substitution effects, and to what extent it impacts upon consumption patterns and producer/retailer responses.109FDEF6, 352380Improve food labellingMajor food manufacturers and supermarkets should agree in the next year a unified system of traffic light food labelling (to be based on percentage of calories for men, women, children and adolescents) and visible calorie indicators for restaurants, especially fast food outlets.565CA4D9, 352381Mandatory health impact assessments for local planning decisionsLocal authority planning decisions should be subject to a mandatory health impact assessment, which would evaluate their potential impact upon the populations’ health.565CA4D9, 352560Existing training is inadequate and ineffectiveTraditional methods of training for healthcare professionals are inadequate and ineffective with respect to obesity.1198CE71, 352713Who should improve obesity training for healthcare professionals?Who should improve systems of obesity education and training across all health professional groups to ensure that all professional primary and secondary healthcare groups are appropriately competent to respond to the demands of the obesity crisis.58D3ABAB, 370328Some clinicians are insensitive in dealing with obese patientsSome clinicians continue to be insensitive, ineffective, and lack confidence when dealing with patients who have problems with their weight.1198CE71, 370330Weight management services are in short supplyThe Academy of Medical Royal Colleges notes that doctors don't have sufficient services available to refer people – that there are a limited number of well-designed fully evidence-based, effective and transferable weight management programmes, available for use in routine NHS primary care.1198CE71, 370331Most obese UK children lack access to weight management programmesThe majority of obese children in the UK don't have access to an evidence-based, proven, multicomponent child weight management programme as recommended by NICE (2006).1198CE71, 370332Early intervention programmesThe investment in weight management services should include greater provision for early intervention programmes.109FDEF6, 370334Weight management service provision is poor in comparison to smokingFrom a clinical perspective, weight management provision needs to mirror the coverage that smoking cessation services have achieved; yet, the investment in smoking cessation programmes remains significantly higher than the investment in weight management programmes. As a comparator, the NHS spent £88.2 million on smoking cessation services in 2011/12.1198CE71, 370335Many healthcare professionals are overweight and obeseDoctors continue to be a trusted and respected source of advice and guidance for patients over their lifestyle choices; however, many healthcare professional struggle with their own weight which can make them less effective both as messengers and exemplars. 1198CE71, 370336Require and examine obesity knowledge as part of curriculaKnowledge, understanding and training in nutrition, physical activity, exercise and the public health aspects of obesity should be an essential part of undergraduate and postgraduate curricula in every discipline because complications of obesity cross all specialty and professional boundaries. This knowledge should be examined. 959C6EF, 370338Weight management services can save more money than they costSome well-designed fully evidence-based, effective and transferable weight management programmes are even economically ‘dominant’ (i.e. they save the NHS more money than it costs to provide the service).1198CE71, 370339Many smaller providers lack formal evidence to support interventionsWhile some of the larger commercial providers have had their efficacy assessed by means of randomised control trials and other evaluative methods, many smaller providers have no such formal evidence to support their interventions.1198CE71, 370342Training should reflect the different needs of different team membersDifferent members of the team will need different training. For example, the role of the GP in an initial consultation differs greatly from that of the bariatric surgeon and his or her team assessing a patient’s suitability for surgery. Different teams need different skills for different patients in different scenarios but healthcare professionals’ education.959C6EF, 370346Training should include sensitive recognition and appropriate referralAll health professionals should have some basic training in sensitive recognition and appropriate referral for overweight and obese patients.959C6EF, 370347NICE guidance has been ignored on bariatric servicesAn investigation by GP newspaper published in December 2014 found that over half of the UK's primary care organisations (PCOs) do not follow NICE or SIGN guidance on bariatric surgery [2].1198CE71, 371449Early years’ intervention is vital to reducing health inequalities1198CE71, 371774Protect and increase green spacesPublic Health England should provide guidance to Directors of Public Health in working with Local Authorities to encourage them to protect or increase green spaces.565CA4D9, 371802Improved engagement and concentrationImproving the food and dining environment for children increases the likelihood that children will be engaged and concentrate in afternoon lessons.1198CE71, 371803Apply mandatory food- and nutrient-based standards to all schoolsThe existing mandatory food- and nutrient-based standards in England should be applied to all schools including free schools and academies.565CA4D9, 371804Require all schools to provide food skills and understandingIntroduce a statutory requirement on all schools to provide food skills, including cooking, and growing, alongside a sound theoretical understanding of the long-term effects of food on health and the environment.565CA4D9, 396117Improve obesity training for healthcare professionalsImprove systems of obesity education and training across all health professional groups to ensure that all professional primary and secondary healthcare groups are appropriately competent to respond to the demands of the obesity crisis.565CA4D9, 399556Improve obesity training for healthcare professionalsImprove systems of obesity education and training across all health professional groups to ensure that all professional primary and secondary healthcare groups are appropriately competent to respond to the demands of the obesity crisis.565CA4D9, 399572Improve food labellingMajor food manufacturers and supermarkets should agree in the next year a unified system of traffic light food labelling (to be based on percentage of calories for men, women, children and adolescents) and visible calorie indicators for restaurants, especially fast food outlets.565CA4D9, 399577Improve nutritional standards for food in hospitalsIntroduce food-based standards—in line with those put in place for schools in England in 2006—in all UK hospitals in the next 18 months; with commissioners working with a delivery agent similar to the Children’s Food Trust to put these measures into place.565CA4D9, 399578Improve nutritional standards in schoolsThe existing mandatory food- and nutrient-based standards in England should be applied to all schools including free schools and academies. This should be accompanied by a new statutory requirement on all schools to provide food skills, including cooking, and growing – alongside a sound theoretical understanding of the long-term effects of food on health and the environment.565CA4D9, 399592Invest in weight management servicesThe departments of health in the four nations should extend and increase the provision of weight management services across the country, to mirror the provision of smoking cessation services.565CA4D9, 399598Mandatory health impact assessments for local planning decisionsLocal authority planning decisions should be subject to a mandatory health impact assessment, which would evaluate their potential impact upon the populations’ health.565CA4D9, 399602Protect and increase green spacesPublic Health England should provide guidance to Directors of Public Health in working with Local Authorities to encourage them to protect or increase green spaces.565CA4D9, 399605Existing training is inadequate and ineffectiveTraditional methods of training for healthcare professionals are inadequate and ineffective with respect to obesity.1198CE71, 399606Who should improve obesity training for healthcare professionals?Improve systems of obesity education and training across all health professional groups to ensure that all professional primary and secondary healthcare groups are appropriately competent to respond to the demands of the obesity crisis.58D3ABAB, 399607Many healthcare professionals are overweight and obeseDoctors continue to be a trusted and respected source of advice and guidance for patients over their lifestyle choices; however, many healthcare professional struggle with their own weight which can make them less effective both as messengers and exemplars. 1198CE71, 399653Increase support for new parentsThe current expansion of the health visitor workforce in England should be accompanied by 'skilling up' the wider early years workforce to deliver basic food preparation skills to new mothers and fathers, and to guide appropriate food choices which will ensure nutritionally balanced meals, encourage breastfeeding and use existing guidance in the Personal Child Health Record as a tool to support this.565CA4D9, 399674Improved engagement and concentrationImproving the food and dining environment for children increases the likelihood that children will be engaged and concentrate in afternoon lessons.1198CE71, 399675Apply mandatory food- and nutrient-based standards to all schoolsThe existing mandatory food- and nutrient-based standards in England should be applied to all schools including free schools and academies.565CA4D9, 399676Require all schools to provide food skills and understandingIntroduce a statutory requirement on all schools to provide food skills, including cooking, and growing, alongside a sound theoretical understanding of the long-term effects of food on health and the environment.565CA4D9, 399677Restrict junk food advertisingBan television advertisements of foods high in saturated fats, sugar and salt before 9pm, and seek agreement with commercial broadcasters not to advertise these foods on internet ‘on-demand’ services. [2]565CA4D9, 399695Focus outcomes indicators on action by primary health professionalsThe Quality Outcomes Framework indicators on obesity should include, and focus on, indicators on the action taken by primary healthcare professionals on behalf of overweight or obese patients. [1]565CA4D9, 399716Weight management services are in short supplyThe Academy of Medical Royal Colleges notes that doctors don't have sufficient services available to refer people – that there are a limited number of well-designed fully evidence-based, effective and transferable weight management programmes, available for use in routine NHS primary care.1198CE71, 399717Most obese UK children lack access to weight management programmesThe majority of obese children in the UK don't have access to an evidence-based, proven, multicomponent child weight management programme as recommended by NICE (2006).1198CE71, 399718Early intervention programmesThe investment in weight management services should include greater provision for early intervention programmes.109FDEF6, 399719Weight management service provision is poor in comparison to smokingFrom a clinical perspective, weight management provision needs to mirror the coverage that smoking cessation services have achieved; yet, the investment in smoking cessation programmes remains significantly higher than the investment in weight management programmes. As a comparator, the NHS spent £88.2 million on smoking cessation services in 2011/12.1198CE71, 399720Weight management services can save more money than they costSome well-designed fully evidence-based, effective and transferable weight management programmes are even economically ‘dominant’ (i.e. they save the NHS more money than it costs to provide the service).1198CE71, 399721Many smaller providers lack formal evidence to support interventionsWhile some of the larger commercial providers have had their efficacy assessed by means of randomised control trials and other evaluative methods, many smaller providers have no such formal evidence to support their interventions.1198CE71, 399735Some clinicians are insensitive in dealing with obese patientsSome clinicians continue to be insensitive, ineffective, and lack confidence when dealing with patients who have problems with their weight.1198CE71, 399738Require and examine obesity knowledge as part of curriculaKnowledge, understanding and training in nutrition, physical activity, exercise and the public health aspects of obesity should be an essential part of undergraduate and postgraduate curricula in every discipline because complications of obesity cross all specialty and professional boundaries. This knowledge should be examined. 959C6EF, 399739Training should reflect the different needs of different team membersDifferent members of the team will need different training. For example, the role of the GP in an initial consultation differs greatly from that of the bariatric surgeon and his or her team assessing a patient’s suitability for surgery. Different teams need different skills for different patients in different scenarios but healthcare professionals’ education.959C6EF, 399740Training should include sensitive recognition and appropriate referralAll health professionals should have some basic training in sensitive recognition and appropriate referral for overweight and obese patients.959C6EF, 399767Early years’ intervention is vital to reducing health inequalities1198CE71, 399777Reduce fast food outlets near schoolsPublic Health England should, in its first 18 months of operation, undertake an audit of local authority licensing and catering arrangements with the intention of developing formal recommendations on reducing the proximity of fast food outlets to schools, colleges, leisure centres and other places where children gather.565CA4D9, 399796NICE guidance has been ignored on bariatric servicesAn investigation by GP newspaper published in December 2014 found that over half of the UK's primary care organisations (PCOs) do not follow NICE or SIGN guidance on bariatric surgery [2].1198CE71, 399872Pilot a 20%+ tax on all sugary, soft drinks for 1 yearFor an initial one year, a duty should be piloted on all sugary soft drinks, increasing the price by at least 20%. This would be an experimental measure, looking at price elasticity, substitution effects, and to what extent it impacts upon consumption patterns and producer/retailer responses.109FDEF6 URL: | | Ištrauka - The Academy of Medical Royal Colleges has called on the departments of health in the four nations to together invest at least £100m in each of the next three financial years to extend and increase provision of weight management services across the country, to mirror the provision of smoking cessation services. |
Link[2] Overcoming obesity: An initial economic analysis
Cituoja: Richard Dobbs, Corinne Sawers, Fraser Thompson, James Manyika - Jonathan Woetzel, Peter Child, Sorcha McKenna, Angela Spatharou (McKinsey Global Institute)
Publication info: 2014 November
Cituojamas: David Price 2:51 PM 10 January 2015 GMT
Citerank: (60) 340964Tackling obesity in the UKWith concern growing that the Foresight analysis—that 50% of the UK population could be obese by 2050, at an annual cost to the nation of around £50 billion per year [2]—substantially underestimates the scale of the unfolding obesity crisis, the College of Contemporary Health is working with the wider policy community to develop a whole systems map of the obesity crisis and the potential responses.7F1CEB7, 348675Adopt a whole systems approach to obesityTackling obesity effectively—accomplishing a population wide-shift—requires a comprehensive and integrated whole systems approach, involving a range of measures focusing on individuals, social and other systems, including at the local and community level, and on the interrelated physical, physiological, social and cognitive factors that determine health outcomes.565CA4D9, 348767A potentially unsustainable financial burden on the health systemThe range of obesity's impacts makes accurate economic analysis challenging; however, a November 2014 study from the McKinsey Global Institute placed the annual economic impact on the UK at around $73bn (£46bn). Earlier analysis and modelling for the 2007 Foresight Report suggested a cost to the NHS of around £4.2bn annually to treat people with health problems related to elevated BMI and a total wider cost to the economy of around £15.8bn (rising to £27bn by 2015 and £49.9bn by 2050).57DE7179, 348770Tackling obesityMany policy interventions have been suggested to address the obesity crisis across multiple studies—and indeed many such measures have been implemented, and are being implemented, now. There's recognition too that these interventions need to be part of a coherent and comprehensive whole systems strategy [4]; with some grounds for optimism that such an approach has the potential to accomplish a significant reduction in the prevalence of obesity in the UK across the next decade. [2]565CA4D9, 348780Causes of obesityUnderstanding the causes of obesity is critical to the success of prevention and treatment strategies. However, while (simply put) obesity occurs when energy intake from food and drink consumption is greater than energy expenditure through the body’s metabolism and physical activity over a prolonged period (resulting in the accumulation of excess body fat), in reality many complex behavioural and societal factors contribute systemically to the current crisis and no single influence dominates.555CD992, 352311Lost productivityObesity has as a serious impact on UK economic development – constraining economic productivity and increasing business costs – affecting individuals’ ability to get and hold down work, their self-esteem and their underlying mental health.57DE7179, 352311Lost productivityObesity has as a serious impact on UK economic development – constraining economic productivity and increasing business costs – affecting individuals’ ability to get and hold down work, their self-esteem and their underlying mental health.57DE7179, 352710Develop better pharmaceutical obesity therapiesObesity drug sales are forecast to $3.8bn globally in 2018 [2]—in comparison to $57bn for Diabetes drug sales[2]—with evidence suggesting that the modest average weight losses achieved with current anti-obesity agents may be of some clinical benefit [5]. However, the current generation of drugs, which act on the central nervous system to suppress appetite, have raised significant health concerns—including psychiatric disorders, such as suicidal behaviour, depression, and cardiovascular problems.565CA4D9, 352718Invest in employee health and wellbeingEncourage organisations to invest employee health and wellbeing; including a health risk assessment and the provision of resources to help employees address the factors that pose the greatest risk to their health and wellness. [1], [2], [3], [4], [5]565CA4D9, 366161McKinsey Global InstituteThe MGI discussion paper, Overcoming obesity: An initial economic analysis studied studied 74 interventions (in 18 areas) that are being discussed or piloted somewhere around the world to address obesity, including subsidized school meals for all, calorie and nutrition labeling, restrictions on advertising high-calorie food and drinks, and public-health campaigns – with sufficient data found on 44 of the interventions in 16 areas. 58D3ABAB, 366169Obesity Interventions identified by MGI74 interventions – across 18 groups – to reduce obesity.565CA4D9, 366449Deploy and integrate as many interventions as possible at scaleCommission and deploy as many interventions as possible at scale and delivered effectively, and integrated way, by the full range of sectors in society.565CA4D9, 366450Understand how to align incentives and build cooperation109FDEF6, 366452No single solution creates sufficient impact to reverse obesityNo single solution creates sufficient impact to reverse obesity: only a comprehensive, systemic program of multiple interventions is likely to be effective. 1198CE71, 366453Many interventions are highly cost-effectiveAlmost all of the interventions we analyzed are highly cost-effective from the viewpoint of society.1198CE71, 366454Education and personal responsibility are necessary but not sufficientEducation and encouraging personal responsibility are necessary but not sufficient.1198CE71, 366456Co-ordinated multi-party actions are required to tackle obesityCapturing the full potential impact is likely to require commitment from government, employers, educators, retailers, restaurants, and food and beverage manufacturers, and a combination of top-down corporate and government interventions and bottom-up community-based ones. 1198CE71, 366457Government obesity efforts are too fragmented to be effectiveGovernment efforts to tackle the obesity issue seem too fragmented to be effective. In the United Kingdom, 15 central government departments; all local authorities with responsibility for health, education, and local planning; 16 EU directorates-general; and a wide range of nongovernmental organizations all have a significant impact on the major intervention areas. [1]118FF4888, 366458Current incentives are mis-aligned118FF4888, 366460Desire to prioritise options becomes a barrier to actionA search for the “best” interventions or a single solution could delay action and displace responsibility. Given the seriousness of the obesity issue, the aim should be to do as much as possible as soon as possible. [1]118FF4888, 366462Experiment with multiple interventionsSociety should be prepared to experiment with possible interventions. In many intervention areas, impact data from high-quality, randomized control trials are not possible to gather. So, rather than waiting for such data, the relevant sectors of society should be pragmatic with a bias toward action, especially where the risks of intervening are low, using trial and error to flesh out their understanding of potential solutions. 565CA4D9, 366463Paucity of investment in intervention measuresThe UK invests less than $1 billion a year in prevention activities such as weight-management programs and public health campaigns – i.e. around 1% of the social cost of obesity in the UK. More investment is required.555CD992, 366467Encourage active transport (walking and cycling)Government authorities redesign urban planning to facilitate and encourage walking and cycling.565CA4D9, 366479Align the school curriculum with obesity, nutrition and activity goals565CA4D9, 366479Align the school curriculum with obesity, nutrition and activity goals565CA4D9, 366481Improve surgical interventions for obesity565CA4D9, 366483Types of weight-management services565CA4D9, 366555Employers offer team challenge incentive schemes in the workplaceEmployers provide team challenge activities to encourage physical activity and improved key health indicators in the workplace.565CA4D9, 366557Employers give employees financial incentives to improve healthEmployers provide material incentives to individuals for improved key health indicators (e.g., discounts on insurance premiums, gym membership, prizes).565CA4D9, 366827Develop a coherent fiscal, regulatory and governance frameworkTake every opportunity, iteratively over time, to bring the public fiscal, regulatory and governance framework into alignment with public health goals on obesity. Use taxes, subsidies, targets and pricing signals to incentivise change in behaviour, supply and consumption by aligning measures with the health properties of food and drink and behaviour—and seek, wherever practical, to amplify positive patterns that are aligned with the policy goals and damp those that pull against.565CA4D9, 371556Many obesity policy measures appear to be cost-effective for societyThe recent MGI study [1] reported that almost all of the obesity policy interventions included in its economic analysis appeared to be highly cost-effective at the societal level—i.e. the health-care costs and productivity savings that accrue from reducing obesity through a specific intervention outweighed the direct investment required to deliver that intervention when assessed over the full lifetime of the target population.1198CE71, 399546Tackling obesityMany policy interventions have been suggested to address the obesity crisis across multiple studies—and indeed many such measures have been implemented, and are being implemented, now. There's recognition too that these interventions need to be part of a coherent and comprehensive whole systems strategy [4]; with some grounds for optimism that such an approach has the potential to accomplish a significant reduction in the prevalence of obesity in the UK across the next decade. [2]565CA4D9, 399547Adopt a whole systems approach to obesityTackling obesity effectively—accomplishing a population wide-shift—requires a comprehensive and integrated whole systems approach, involving a range of measures focusing on individuals, social and other systems, including at the local and community level, and on the interrelated physical, physiological, social and cognitive factors that determine health outcomes.565CA4D9, 399548Invest in employee health and wellbeingEncourage organisations to invest employee health and wellbeing; including a health risk assessment and the provision of resources to help employees address the factors that pose the greatest risk to their health and wellness. [1], [2], [3], [4], [5]565CA4D9, 399552Develop a coherent fiscal, regulatory and governance frameworkTake every opportunity, iteratively over time, to bring the public fiscal, regulatory and governance framework into alignment with public health goals on obesity. Use taxes, subsidies, targets and pricing signals to incentivise change in behaviour, supply and consumption by aligning measures with the health properties of food and drink and behaviour—and seek, wherever practical, to amplify positive patterns that are aligned with the policy goals and damp those that pull against.565CA4D9, 399555Many obesity policy measures appear to be cost-effective for societyThe recent MGI study [1] reported that almost all of the obesity policy interventions included in its economic analysis appeared to be highly cost-effective at the societal level—i.e. the health-care costs and productivity savings that accrue from reducing obesity through a specific intervention outweighed the direct investment required to deliver that intervention when assessed over the full lifetime of the target population.1198CE71, 399561Deploy and integrate as many interventions as possible at scaleCommission and deploy as many interventions as possible at scale and delivered effectively, and integrated way, by the full range of sectors in society.565CA4D9, 399567Employers offer team challenge incentive schemes in the workplaceEmployers provide team challenge activities to encourage physical activity and improved key health indicators in the workplace.565CA4D9, 399568Employers give employees financial incentives to improve healthEmployers provide material incentives to individuals for improved key health indicators (e.g., discounts on insurance premiums, gym membership, prizes).565CA4D9, 399575Align the school curriculum with obesity, nutrition and activity goals565CA4D9, 399575Align the school curriculum with obesity, nutrition and activity goals565CA4D9, 399586Develop better pharmaceutical obesity therapiesObesity drug sales are forecast to $3.8bn globally in 2018 [2]—in comparison to $57bn for Diabetes drug sales[2]—with evidence suggesting that the modest average weight losses achieved with current anti-obesity agents may be of some clinical benefit [5]. However, the current generation of drugs, which act on the central nervous system to suppress appetite, have raised significant health concerns—including psychiatric disorders, such as suicidal behaviour, depression, and cardiovascular problems.565CA4D9, 399588Improve surgical interventions for obesity565CA4D9, 399592Invest in weight management servicesThe departments of health in the four nations should extend and increase the provision of weight management services across the country, to mirror the provision of smoking cessation services.565CA4D9, 399599Encourage active transport (walking and cycling)Government authorities redesign urban planning to facilitate and encourage walking and cycling.565CA4D9, 399611Understand how to align incentives and build cooperation109FDEF6, 399612Co-ordinated multi-party actions are required to tackle obesityCapturing the full potential impact is likely to require commitment from government, employers, educators, retailers, restaurants, and food and beverage manufacturers, and a combination of top-down corporate and government interventions and bottom-up community-based ones. 1198CE71, 399613No single solution creates sufficient impact to reverse obesityNo single solution creates sufficient impact to reverse obesity: only a comprehensive, systemic program of multiple interventions is likely to be effective. 1198CE71, 399614Many interventions are highly cost-effectiveAlmost all of the interventions we analyzed are highly cost-effective from the viewpoint of society.1198CE71, 399615Education and personal responsibility are necessary but not sufficientEducation and encouraging personal responsibility are necessary but not sufficient.1198CE71, 399617Experiment with multiple interventionsSociety should be prepared to experiment with possible interventions. In many intervention areas, impact data from high-quality, randomized control trials are not possible to gather. So, rather than waiting for such data, the relevant sectors of society should be pragmatic with a bias toward action, especially where the risks of intervening are low, using trial and error to flesh out their understanding of potential solutions. 565CA4D9, 399715Types of weight-management services565CA4D9, 399887Causes of obesityUnderstanding the causes of obesity is critical to the success of prevention and treatment strategies. However, while (simply put) obesity occurs when energy intake from food and drink consumption is greater than energy expenditure through the body’s metabolism and physical activity over a prolonged period (resulting in the accumulation of excess body fat), in reality many complex behavioural and societal factors contribute systemically to the current crisis and no single influence dominates.555CD992, 399932Paucity of investment in intervention measuresThe UK invests less than $1 billion a year in prevention activities such as weight-management programs and public health campaigns – i.e. around 1% of the social cost of obesity in the UK. More investment is required.555CD992, 399973A potentially unsustainable financial burden on the health systemThe range of obesity's impacts makes accurate economic analysis challenging; however, a November 2014 study from the McKinsey Global Institute placed the annual economic impact on the UK at around $73bn (£46bn). Earlier analysis and modelling for the 2007 Foresight Report suggested a cost to the NHS of around £4.2bn annually to treat people with health problems related to elevated BMI and a total wider cost to the economy of around £15.8bn (rising to £27bn by 2015 and £49.9bn by 2050).57DE7179, 400018Lost productivityObesity has as a serious impact on UK economic development – constraining economic productivity and increasing business costs – affecting individuals’ ability to get and hold down work, their self-esteem and their underlying mental health.57DE7179, 400018Lost productivityObesity has as a serious impact on UK economic development – constraining economic productivity and increasing business costs – affecting individuals’ ability to get and hold down work, their self-esteem and their underlying mental health.57DE7179, 400061Current incentives are mis-aligned118FF4888, 400083Government obesity efforts are too fragmented to be effectiveGovernment efforts to tackle the obesity issue seem too fragmented to be effective. In the United Kingdom, 15 central government departments; all local authorities with responsibility for health, education, and local planning; 16 EU directorates-general; and a wide range of nongovernmental organizations all have a significant impact on the major intervention areas.118FF4888, 400084Desire to priortise options becomes a barrier to actionA search for the “best” interventions or a single solution could delay action and displace responsibility. Given the seriousness of the obesity issue, the aim should be to do as much as possible as soon as possible.118FF4888 URL:
|
|
|