|
![]()
| Invest in employee health and wellbeing How1 #352718 Encourage organisations to invest employee health and wellbeing; including a health risk assessment and the provision of resources to help employees address the factors that pose the greatest risk to their health and wellness. [1], [2], [3], [4], [5] | 1. Employers should encourage healthy eating among staff by: • implementing the National Institute for Health and Clinical Excellence (NICE) recommendations for obesity in the workplace (NICE CG43) [2] • ensuring that healthy food is available in the workplace at affordable or subsidised prices • encouraging nutritional labelling to allow employees to make informed food choices • setting strict nutritional criteria as part of procurement contracts for food made available in food outlets and vending machines. 2. Employers should encourage physical activity by: • signposting to and encouraging the use of walking and cycling routes and stairs, including the provision of safe cycle storage areas • recommending the use of active travel methods to and from work, and provision of changing room facilities • working with local authorities to enhance access to health services by public transport • considering the use of staff incentives such as discounted membership of fitness clubs. 3. Employers should encourage healthy behaviour change by: • developing a strategy for staff health and wellbeing • encouraging staff to take regular breaks to move around as well as sufficient time to eat well • using innovative ways to encourage lifestyle change amongst staff, e.g. intranet messages on health, and signposting local activity/weight management opportunities • using staff training as an opportunity to ensure that leaders are aware of the importance of encouraging proactive approaches to staff health • enabling equitable staff access to a range of weight management and activity options, by commissioning weight management services which have proven effectiveness. 4. Occupational health departments have a responsibility to diagnose overweight and obesity in new employees, and wherever employees make health contacts (eg winter influenza vaccination) to communicate the health benefits of weight loss, and signpost obese employees either to ‘in-house’ or community-based services. Occupational health services could contribute to the monitoring of those engaged in weight management programmes by providing weighing facilities and information on healthy eating and activity opportunities within and outside the workplace. Cost-effective interventions to reduce obesity in the UK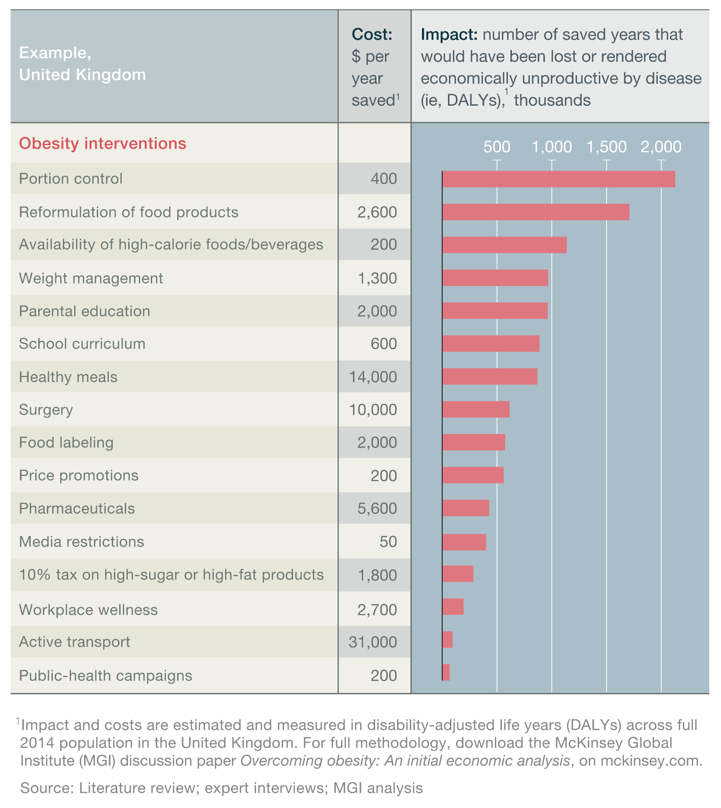 |
+Citations (7) - CitationsAjouter une citationList by: CiterankMapLink[1] Action on obesity: Comprehensive care for all
En citant: Royal College of Physicians
Publication info: 2013 January
Cité par: David Price 8:26 AM 9 September 2014 GMT
Citerank: (46) 348686Improve support for people with severe and complicated obesityGreater focus needs to be devoted to strategies supporting individuals who are already obese. Current government policy is focused largely on prevention, which is vital in ensuring the scale of the obesity problem and its associated costs do not increase. It does not, however, address the problems of those people already obese or morbidly obese and the costs associated with their health conditions. Moreover, obesity treatment is often cost effective.109FDEF6, 3523581 in 5 UK children aged 10-11 are obeseThe National Child Measurement Programme (NCMP) figures for 2013/14, show that 19.1% of children in Year 6 (aged 10-11) were obese and a further 14.4% were overweight. Obese children and adolescents are at an increased risk of developing various health problems—such as asthma, cardiovascular disease and type 2 diabetes (as well as low self-esteem and depression)—and are also more likely to become obese adults.648CC79C, 352454What is obesity?Obesity is a medical condition in which excess body fat has accumulated to the extent that it may result in increased health problems and reduced life expectancy. As central obesity (excess ectopic fat stored around major organs and abdomen) is the most dangerous form to health, waist measurement can be a key indicator of risk. Generally, men with a waist circumference of 94cm or more (and women of 80cm or more) are more likely to develop obesity-related health problems.82AECCD8, 352559Weight management services in the UK are poorly developedAlthough the prevalence of obesity in adults and in children in the UK is amongst the highest in the developed world, the multidisciplinary services necessary to manage patients with an established problem of excess weight and its clinical consequences are poorly developed within the UK. Some prevention and intervention strategies are provided in primary care, but secondary care and specialist services remain underdeveloped or unavailable to meet the need.555CD992, 352560Existing training is inadequate and ineffectiveTraditional methods of training for healthcare professionals are inadequate and ineffective with respect to obesity.1198CE71, 352562Multidisciplinary teams to cover severe and complex obesity across UKCommissioning of specialist obesity services should be for multidisciplinary care of ‘severe and complex obesity’ and not directly for rather than just bariatric surgical treatment. Need multidisciplinary teams (MDTs) available to cover severe and complex obesity throughout the UK.109FDEF6, 352563Increase investment in obesity research565CA4D9, 352564Every local authority should have an obesity champion565CA4D9, 352565Better weight management resources for obese healthcare workersBetter weight management resources for healthcare workers who have an obesity problem.565CA4D9, 352566Set up a specialist group of bariatric nursesThe Royal College of Physicians in conjunction with the Royal College of Nursing should up a specialist group of bariatric nurses who are trained in the specialist aspects of bariatric medicine and surgery, including post-surgery follow-up.565CA4D9, 352569Develop a patient charter for those with obesity problems109FDEF6, 352570Undertake a systematic review of specialist obesity servicesUndertake a systematic review of specialist obesity services between the Royal College of General Practitioners community leads and the Royal College of Physicians (RCP) and learned societies, including the Society for Endocrinology, Diabetes UK and the Association of British Clinical Diabetologists565CA4D9, 352589RCP oversee the development of multidisciplinary bariatric servicesThe Royal College of Physicians (RCP) should oversee the development of multidisciplinary bariatric services to cover the population in the UK.109FDEF6, 352590RCP should provide courses to train doctors in MDT formationThe RCP should promote the provision of these multidisciplinary groups by developing and providing courses that advise, encourage and train doctors (and other healthcare professionals) on their formation.109FDEF6, 352713Who should improve obesity training for healthcare professionals?Who should improve systems of obesity education and training across all health professional groups to ensure that all professional primary and secondary healthcare groups are appropriately competent to respond to the demands of the obesity crisis.58D3ABAB, 352714Pharmacological treatment can be cost-effectiveA systematic review of pharmacological treatment in primary care (orlistat, sibutramine and rimonabant– the latter two now withdrawn) has shown all were effective at reducing weight and BMI, and cost effective when using a threshold of £20,000 per QALY. 1198CE71, 352716Bariatric surgery can be cost effectiveAnalysis by the Office of Health Economics estimated that between around 10,000 and 140,000 of patients could receive bariatric surgery based on the assumption of between 1% and 25% of patients eligible for surgery choosing to take this option. Overall the economic benefit ranged between £382m and £1,295m savings after three years to the NHS after surgery if 25% of patients potentially eligible for surgery chose this option.1198CE71, 352913Royal College of PhysiciansIn addition to supporting physicians in their daily practice, our public health activities include campaigning for change, advising government and parliament, and taking part in national debates on medical, clinical and public health issues. The RCP has supported and represented physicians for nearly 500 years. Our roots stretch back to Henry VIII, but our 29,000 members today work in the fast-paced, ever-changing, highly technological world of medicine in the UK and across the globe.58D3ABAB, 362143Appoint an obesity champion or tsarAppoint a government obesity champion to drive a coordinated obesity strategy between and across central government departments which include Health, the Treasury, Sport, Education, Agriculture, the Department of Work and Pensions, and local government for the local environment. This person should have a strong but politically independent status (e.g. a member of the House of Lords) with the skills and authority to address issues which need multiple government departmental involvement.565CA4D9, 370326Many health professionals still have inadequate knowledgeMany recently trained health professionals still have an inadequate knowledge of the nutritional aspects of health promotion and disease treatment and the potential benefits of regular physical activity.1198CE71, 370327Understand the ten essential facts about obesityAll healthcare professionals should know and understand the ‘Ten essential facts about obesity’.109FDEF6, 371613Strong business case for investment in employee health and wellbeingInvesting in the health and wellbeing of employees makes business sense. It has been estimated that working age ill-health costs the UK £100 billion per annum, more than the annual budget for the NHS. In 2009–10, 23.4 million days were lost due to work-related ill-health.1198CE71, 396117Improve obesity training for healthcare professionalsImprove systems of obesity education and training across all health professional groups to ensure that all professional primary and secondary healthcare groups are appropriately competent to respond to the demands of the obesity crisis.565CA4D9, 399548Invest in employee health and wellbeingEncourage organisations to invest employee health and wellbeing; including a health risk assessment and the provision of resources to help employees address the factors that pose the greatest risk to their health and wellness. [1], [2], [3], [4], [5]565CA4D9, 399556Improve obesity training for healthcare professionalsImprove systems of obesity education and training across all health professional groups to ensure that all professional primary and secondary healthcare groups are appropriately competent to respond to the demands of the obesity crisis.565CA4D9, 399564Better weight management resources for obese healthcare workersBetter weight management resources for healthcare workers who have an obesity problem.565CA4D9, 399569Strong business case for investment in employee health and wellbeingInvesting in the health and wellbeing of employees makes business sense. It has been estimated that working age ill-health costs the UK £100 billion per annum, more than the annual budget for the NHS. In 2009–10, 23.4 million days were lost due to work-related ill-health.1198CE71, 399585Undertake a systematic review of specialist obesity servicesUndertake a systematic review of specialist obesity services between the Royal College of General Practitioners community leads and the Royal College of Physicians (RCP) and learned societies, including the Society for Endocrinology, Diabetes UK and the Association of British Clinical Diabetologists565CA4D9, 399593Increase investment in obesity research565CA4D9, 399605Existing training is inadequate and ineffectiveTraditional methods of training for healthcare professionals are inadequate and ineffective with respect to obesity.1198CE71, 399606Who should improve obesity training for healthcare professionals?Improve systems of obesity education and training across all health professional groups to ensure that all professional primary and secondary healthcare groups are appropriately competent to respond to the demands of the obesity crisis.58D3ABAB, 399619Appoint an obesity champion or tsarAppoint a government obesity champion to drive a coordinated obesity strategy between and across central government departments which include Health, the Treasury, Sport, Education, Agriculture, the Department of Work and Pensions, and local government for the local environment. This person should have a strong but politically independent status (e.g. a member of the House of Lords) with the skills and authority to address issues which need multiple government departmental involvement.565CA4D9, 399699Set up a a specialist group of bariatric nursesThe Royal College of Physicians in conjunction with the Royal College of Nursing should up a specialist group of bariatric nurses who are trained in the specialist aspects of bariatric medicine and surgery, including post-surgery follow-up.565CA4D9, 399713Improve support for people with severe and complicated obesityGreater focus needs to be devoted to strategies supporting individuals who are already obese. Current government policy is focused largely on prevention, which is vital in ensuring the scale of the obesity problem and its associated costs do not increase. It does not, however, address the problems of those people already obese or morbidly obese and the costs associated with their health conditions. Moreover, obesity treatment is often cost effective.109FDEF6, 399734Many health professionals still have inadequate knowledgeMany recently trained health professionals still have an inadequate knowledge of the nutritional aspects of health promotion and disease treatment and the potential benefits of regular physical activity.1198CE71, 399742Every local authority should have an obesity champion565CA4D9, 399792Multidisciplinary teams to cover severe and complex obesity across UKCommissioning of specialist obesity services should be for multidisciplinary care of ‘severe and complex obesity’ and not directly for rather than just bariatric surgical treatment. Need multidisciplinary teams (MDTs) available to cover severe and complex obesity throughout the UK.109FDEF6, 399793Develop a patient charter for those with obesity problems109FDEF6, 399794Pharmacological treatment can be cost-effectiveA systematic review of pharmacological treatment in primary care (orlistat, sibutramine and rimonabant– the latter two now withdrawn) has shown all were effective at reducing weight and BMI, and cost effective when using a threshold of £20,000 per QALY. 1198CE71, 399795Bariatric surgery can be cost effectiveAnalysis by the Office of Health Economics estimated that between around 10,000 and 140,000 of patients could receive bariatric surgery based on the assumption of between 1% and 25% of patients eligible for surgery choosing to take this option. Overall the economic benefit ranged between £382m and £1,295m savings after three years to the NHS after surgery if 25% of patients potentially eligible for surgery chose this option.1198CE71, 399833Understand the ten essential facts about obesityAll healthcare professionals should know and understand the ‘Ten essential facts about obesity’.109FDEF6, 399859RCP oversee the development of multidisciplinary bariatric servicesThe Royal College of Physicians (RCP) should oversee the development of multidisciplinary bariatric services to cover the population in the UK.109FDEF6, 399860RCP should provide courses to train doctors in MDT formationThe RCP should promote the provision of these multidisciplinary groups by developing and providing courses that advise, encourage and train doctors (and other healthcare professionals) on their formation.109FDEF6, 399892What is obesity?Obesity is a medical condition in which excess body fat has accumulated to the extent that it may result in increased health problems and reduced life expectancy. As central obesity (excess ectopic fat stored around major organs and abdomen) is the most dangerous form to health, waist measurement can be a key indicator of risk. Generally, men with a waist circumference of 94cm or more (and women of 80cm or more) are more likely to develop obesity-related health problems.82AECCD8, 399931Weight management services in the UK are poorly developedAlthough the prevalence of obesity in adults and in children in the UK is amongst the highest in the developed world, the multidisciplinary services necessary to manage patients with an established problem of excess weight and its clinical consequences are poorly developed within the UK. Some prevention and intervention strategies are provided in primary care, but secondary care and specialist services remain underdeveloped or unavailable to meet the need.555CD992, 3999751 in 5 UK children aged 10-11 are obeseThe National Child Measurement Programme (NCMP) figures for 2013/14, show that 19.1% of children in Year 6 (aged 10-11) were obese and a further 14.4% were overweight. Obese children and adolescents are at an increased risk of developing various health problems—such as asthma, cardiovascular disease and type 2 diabetes (as well as low self-esteem and depression)—and are also more likely to become obese adults.648CC79C URL:
|
Link[2] Obesity: Guidance on the prevention of overweight and obesity in adults and children
En citant: NICE - CG43
Cité par: David Price 10:59 AM 5 January 2015 GMT
Citerank: (31) 352351Increased risk of Type 2 diabetes Obesity substantially raises the risk of Type 2 diabetes—with excess body fat estimated to underlie almost two-thirds of cases of diabetes in men and three quarters of cases in women—and people at risk of diabetes can cut their chances of getting diabetes by 60% if they lose between 5% and 7% of their body weight. Worldwide, the number of people with diabetes has tripled since 1985. [2]57DE7179, 369907NICE Guidance on Diet, Nutrition and ObesityNote: extended excerpts from National Institute for Health and Care Excellence are included and cross-linked here to help explore and understand their intersection with the policy space and their implications. Those seeking specific guidance should refer to the full Guidelines and Pathways directly.565CA4D9, 369908NICE – DietHaving a healthy balanced diet helps prevent obesity, cardiovascular and many other conditions. This pathway covers recommendations for everyone about diet and lifestyle, and recommendations for health professionals on interventions to encourage people to follow a healthy diet.565CA4D9, 369909NICE – Lifestyle weight management for overweight or obese adultsLocal authorities, working with other local service providers, clinical commissioning groups and health and wellbeing boards, should ensure there is an integrated approach to preventing and managing obesity and its associated conditions.565CA4D9, 369912NICE – ObesityGuidelines on preventing and managing obesity.565CA4D9, 369913NICE – Obesity working with local communitiesThis pathway focuses on an overarching approach to overweight and obese adults and overweight and obese children in local communities. It focuses on the importance of integrating action on obesity in other local agendas (such as initiatives to prevent type 2 diabetes, cardiovascular disease and cancers, or initiatives to improve the environment and promote sustainability), and provides an organisational framework for the relevant community-based or individual interventions.565CA4D9, 369921NICE – Keeping track of weightEveryone should aim to maintain or achieve a healthy weight, to improve their health and reduce the risk of diseases associated with being overweight and obese, such as coronary heart disease, type 2 diabetes, osteoarthritis and some cancers. Periodically check your weight, waist measurement or a simple alternative, such as the fit of your clothes.565CA4D9, 369923NICE – Diet to maintain a healthy weightBalancing 'calories in' (from food and drink) and 'calories out' (from being physically active) may help to maintain a healthy weight.565CA4D9, 369924NICE – Activity to maintain a healthy weightBalancing 'calories in' (from food and drink) and 'calories out' (from being physically active) may help to maintain a healthy weight.565CA4D9, 369925 NICE – Additional advice for parents and carersIn addition to the general recommendations on behaviours to maintain a healthy weight, the advice below will help children establish healthy behaviours and maintain or work towards a healthy weight. These strategies may have other benefits – for example, monitoring the amount of time children spend watching television may help reduce their exposure to inappropriate programmes or advertisements.565CA4D9, 369926NICE – Advice for adults who wish to lose weightSee also the NICE guidance on diet and activity to maintain a healthy weight.565CA4D9, 369928NICE – Local authority environmental interventions565CA4D9, 369929NICE – Healthcare professional interventionsInterventions by healthcare professional to address obesity.565CA4D9, 369931NICE – Interventions to support smoking cessation All interventions to support smoking cessation should: ensure people are given information on services that provide advice on prevention and management of obesity if appropriate?, and give people who are concerned about their weight general advice on long-term weight management, in particular encouraging increased physical activity.565CA4D9, 369934NICE – Workplace interventionsAll workplaces, particularly large organisations such as the NHS and local authorities should address the prevention and management of obesity, because of the considerable impact on the health of the workforce and associated costs to industry. 565CA4D9, 369937Local authorities and the NHS as employersLocal authorities and the NHS as employers should set an example in developing public health policies to prevent and manage obesity by following existing guidance and (in England) the local obesity strategy.565CA4D9, 369941NICE – School interventions565CA4D9, 370053Standards for take-aways and other food outletsFood from take-aways and other outlets (the 'informal eating out sector') comprises a significant part of many people's diet. Local planning authorities have powers to control fast-food outlets565CA4D9, 370058Supporting people who are stopping smokingAll interventions to support smoking cessation should: (1) ensure people are given information on services that provide advice on prevention and management of obesity, and (2) if appropriate give people who are concerned about their weight general advice on long-term weight management, in particular encouraging increased physical activity.565CA4D9, 370062Lifestyle advice on diet & physical activity for families and children565CA4D9, 370063Diet in early years education and childcareHelp children and young people to have a healthy diet and lifestyle. This includes helping them to develop positive, life-long habits in relation to food. This can be achieved by ensuring the messages conveyed about food, the food and drink available – and where it is consumed – is conducive to a healthy diet.565CA4D9, 370074Training for programme for lifestyle weight management services staff 565CA4D9, 370163Primary Care565CA4D9, 370164Community based programmes and interventions565CA4D9, 370177Training for health and other professionals565CA4D9, 370560Clinical Commissioning GroupsClinical commissioning groups (CCGs) are responsible for commissioning a range of healthcare services for children and adults. This includes specialist obesity services (sometimes called tier 3 services). The groups do not directly commission lifestyle weight management services (sometimes called tier 2 services). Rather, they work with local authorities to coordinate and integrate planning and commissioning through the health and wellbeing board.58D3ABAB, 370918NICE – Interventions to increase physical activity565CA4D9, 370963NICE – Preschool Interventions565CA4D9, 371184NICE – Physical activity in the workplacePhysical activity programmes in the workplace including active travel.565CA4D9, 399548Invest in employee health and wellbeingEncourage organisations to invest employee health and wellbeing; including a health risk assessment and the provision of resources to help employees address the factors that pose the greatest risk to their health and wellness. [1], [2], [3], [4], [5]565CA4D9, 399987Increased risk of Type 2 diabetes Obesity substantially raises the risk of Type 2 diabetes—with excess body fat estimated to underly almost two-thirds of cases of diabetes in men and three quarters of cases in women—and people at risk of diabetes can cut their chances of getting diabetes by 60% if they lose between 5% and 7% of their body weight. Worldwide, the number of people with diabetes has tripled since 1985.57DE7179 URL: |
Link[4] Overcoming obesity: An initial economic analysis
En citant: Richard Dobbs, Corinne Sawers, Fraser Thompson, James Manyika - Jonathan Woetzel, Peter Child, Sorcha McKenna, Angela Spatharou (McKinsey Global Institute)
Publication info: 2014 November
Cité par: David Price 11:02 AM 5 January 2015 GMT
Citerank: (60) 340964Tackling obesity in the UKWith concern growing that the Foresight analysis—that 50% of the UK population could be obese by 2050, at an annual cost to the nation of around £50 billion per year [2]—substantially underestimates the scale of the unfolding obesity crisis, the College of Contemporary Health is working with the wider policy community to develop a whole systems map of the obesity crisis and the potential responses.7F1CEB7, 348675Adopt a whole systems approach to obesityTackling obesity effectively—accomplishing a population wide-shift—requires a comprehensive and integrated whole systems approach, involving a range of measures focusing on individuals, social and other systems, including at the local and community level, and on the interrelated physical, physiological, social and cognitive factors that determine health outcomes.565CA4D9, 348767A potentially unsustainable financial burden on the health systemThe range of obesity's impacts makes accurate economic analysis challenging; however, a November 2014 study from the McKinsey Global Institute placed the annual economic impact on the UK at around $73bn (£46bn). Earlier analysis and modelling for the 2007 Foresight Report suggested a cost to the NHS of around £4.2bn annually to treat people with health problems related to elevated BMI and a total wider cost to the economy of around £15.8bn (rising to £27bn by 2015 and £49.9bn by 2050).57DE7179, 348770Tackling obesityMany policy interventions have been suggested to address the obesity crisis across multiple studies—and indeed many such measures have been implemented, and are being implemented, now. There's recognition too that these interventions need to be part of a coherent and comprehensive whole systems strategy [4]; with some grounds for optimism that such an approach has the potential to accomplish a significant reduction in the prevalence of obesity in the UK across the next decade. [2]565CA4D9, 348780Causes of obesityUnderstanding the causes of obesity is critical to the success of prevention and treatment strategies. However, while (simply put) obesity occurs when energy intake from food and drink consumption is greater than energy expenditure through the body’s metabolism and physical activity over a prolonged period (resulting in the accumulation of excess body fat), in reality many complex behavioural and societal factors contribute systemically to the current crisis and no single influence dominates.555CD992, 352311Lost productivityObesity has as a serious impact on UK economic development – constraining economic productivity and increasing business costs – affecting individuals’ ability to get and hold down work, their self-esteem and their underlying mental health.57DE7179, 352311Lost productivityObesity has as a serious impact on UK economic development – constraining economic productivity and increasing business costs – affecting individuals’ ability to get and hold down work, their self-esteem and their underlying mental health.57DE7179, 352373Invest in weight management servicesThe departments of health in the four nations should extend and increase the provision of weight management services across the country, to mirror the provision of smoking cessation services.565CA4D9, 352710Develop better pharmaceutical obesity therapiesObesity drug sales are forecast to $3.8bn globally in 2018 [2]—in comparison to $57bn for Diabetes drug sales[2]—with evidence suggesting that the modest average weight losses achieved with current anti-obesity agents may be of some clinical benefit [5]. However, the current generation of drugs, which act on the central nervous system to suppress appetite, have raised significant health concerns—including psychiatric disorders, such as suicidal behaviour, depression, and cardiovascular problems.565CA4D9, 366161McKinsey Global InstituteThe MGI discussion paper, Overcoming obesity: An initial economic analysis studied studied 74 interventions (in 18 areas) that are being discussed or piloted somewhere around the world to address obesity, including subsidized school meals for all, calorie and nutrition labeling, restrictions on advertising high-calorie food and drinks, and public-health campaigns – with sufficient data found on 44 of the interventions in 16 areas. 58D3ABAB, 366169Obesity Interventions identified by MGI74 interventions – across 18 groups – to reduce obesity.565CA4D9, 366449Deploy and integrate as many interventions as possible at scaleCommission and deploy as many interventions as possible at scale and delivered effectively, and integrated way, by the full range of sectors in society.565CA4D9, 366450Understand how to align incentives and build cooperation109FDEF6, 366452No single solution creates sufficient impact to reverse obesityNo single solution creates sufficient impact to reverse obesity: only a comprehensive, systemic program of multiple interventions is likely to be effective. 1198CE71, 366453Many interventions are highly cost-effectiveAlmost all of the interventions we analyzed are highly cost-effective from the viewpoint of society.1198CE71, 366454Education and personal responsibility are necessary but not sufficientEducation and encouraging personal responsibility are necessary but not sufficient.1198CE71, 366456Co-ordinated multi-party actions are required to tackle obesityCapturing the full potential impact is likely to require commitment from government, employers, educators, retailers, restaurants, and food and beverage manufacturers, and a combination of top-down corporate and government interventions and bottom-up community-based ones. 1198CE71, 366457Government obesity efforts are too fragmented to be effectiveGovernment efforts to tackle the obesity issue seem too fragmented to be effective. In the United Kingdom, 15 central government departments; all local authorities with responsibility for health, education, and local planning; 16 EU directorates-general; and a wide range of nongovernmental organizations all have a significant impact on the major intervention areas. [1]118FF4888, 366458Current incentives are mis-aligned118FF4888, 366460Desire to prioritise options becomes a barrier to actionA search for the “best” interventions or a single solution could delay action and displace responsibility. Given the seriousness of the obesity issue, the aim should be to do as much as possible as soon as possible. [1]118FF4888, 366462Experiment with multiple interventionsSociety should be prepared to experiment with possible interventions. In many intervention areas, impact data from high-quality, randomized control trials are not possible to gather. So, rather than waiting for such data, the relevant sectors of society should be pragmatic with a bias toward action, especially where the risks of intervening are low, using trial and error to flesh out their understanding of potential solutions. 565CA4D9, 366463Paucity of investment in intervention measuresThe UK invests less than $1 billion a year in prevention activities such as weight-management programs and public health campaigns – i.e. around 1% of the social cost of obesity in the UK. More investment is required.555CD992, 366467Encourage active transport (walking and cycling)Government authorities redesign urban planning to facilitate and encourage walking and cycling.565CA4D9, 366479Align the school curriculum with obesity, nutrition and activity goals565CA4D9, 366479Align the school curriculum with obesity, nutrition and activity goals565CA4D9, 366481Improve surgical interventions for obesity565CA4D9, 366483Types of weight-management services565CA4D9, 366555Employers offer team challenge incentive schemes in the workplaceEmployers provide team challenge activities to encourage physical activity and improved key health indicators in the workplace.565CA4D9, 366557Employers give employees financial incentives to improve healthEmployers provide material incentives to individuals for improved key health indicators (e.g., discounts on insurance premiums, gym membership, prizes).565CA4D9, 366827Develop a coherent fiscal, regulatory and governance frameworkTake every opportunity, iteratively over time, to bring the public fiscal, regulatory and governance framework into alignment with public health goals on obesity. Use taxes, subsidies, targets and pricing signals to incentivise change in behaviour, supply and consumption by aligning measures with the health properties of food and drink and behaviour—and seek, wherever practical, to amplify positive patterns that are aligned with the policy goals and damp those that pull against.565CA4D9, 371556Many obesity policy measures appear to be cost-effective for societyThe recent MGI study [1] reported that almost all of the obesity policy interventions included in its economic analysis appeared to be highly cost-effective at the societal level—i.e. the health-care costs and productivity savings that accrue from reducing obesity through a specific intervention outweighed the direct investment required to deliver that intervention when assessed over the full lifetime of the target population.1198CE71, 399546Tackling obesityMany policy interventions have been suggested to address the obesity crisis across multiple studies—and indeed many such measures have been implemented, and are being implemented, now. There's recognition too that these interventions need to be part of a coherent and comprehensive whole systems strategy [4]; with some grounds for optimism that such an approach has the potential to accomplish a significant reduction in the prevalence of obesity in the UK across the next decade. [2]565CA4D9, 399547Adopt a whole systems approach to obesityTackling obesity effectively—accomplishing a population wide-shift—requires a comprehensive and integrated whole systems approach, involving a range of measures focusing on individuals, social and other systems, including at the local and community level, and on the interrelated physical, physiological, social and cognitive factors that determine health outcomes.565CA4D9, 399548Invest in employee health and wellbeingEncourage organisations to invest employee health and wellbeing; including a health risk assessment and the provision of resources to help employees address the factors that pose the greatest risk to their health and wellness. [1], [2], [3], [4], [5]565CA4D9, 399552Develop a coherent fiscal, regulatory and governance frameworkTake every opportunity, iteratively over time, to bring the public fiscal, regulatory and governance framework into alignment with public health goals on obesity. Use taxes, subsidies, targets and pricing signals to incentivise change in behaviour, supply and consumption by aligning measures with the health properties of food and drink and behaviour—and seek, wherever practical, to amplify positive patterns that are aligned with the policy goals and damp those that pull against.565CA4D9, 399555Many obesity policy measures appear to be cost-effective for societyThe recent MGI study [1] reported that almost all of the obesity policy interventions included in its economic analysis appeared to be highly cost-effective at the societal level—i.e. the health-care costs and productivity savings that accrue from reducing obesity through a specific intervention outweighed the direct investment required to deliver that intervention when assessed over the full lifetime of the target population.1198CE71, 399561Deploy and integrate as many interventions as possible at scaleCommission and deploy as many interventions as possible at scale and delivered effectively, and integrated way, by the full range of sectors in society.565CA4D9, 399567Employers offer team challenge incentive schemes in the workplaceEmployers provide team challenge activities to encourage physical activity and improved key health indicators in the workplace.565CA4D9, 399568Employers give employees financial incentives to improve healthEmployers provide material incentives to individuals for improved key health indicators (e.g., discounts on insurance premiums, gym membership, prizes).565CA4D9, 399575Align the school curriculum with obesity, nutrition and activity goals565CA4D9, 399575Align the school curriculum with obesity, nutrition and activity goals565CA4D9, 399586Develop better pharmaceutical obesity therapiesObesity drug sales are forecast to $3.8bn globally in 2018 [2]—in comparison to $57bn for Diabetes drug sales[2]—with evidence suggesting that the modest average weight losses achieved with current anti-obesity agents may be of some clinical benefit [5]. However, the current generation of drugs, which act on the central nervous system to suppress appetite, have raised significant health concerns—including psychiatric disorders, such as suicidal behaviour, depression, and cardiovascular problems.565CA4D9, 399588Improve surgical interventions for obesity565CA4D9, 399592Invest in weight management servicesThe departments of health in the four nations should extend and increase the provision of weight management services across the country, to mirror the provision of smoking cessation services.565CA4D9, 399599Encourage active transport (walking and cycling)Government authorities redesign urban planning to facilitate and encourage walking and cycling.565CA4D9, 399611Understand how to align incentives and build cooperation109FDEF6, 399612Co-ordinated multi-party actions are required to tackle obesityCapturing the full potential impact is likely to require commitment from government, employers, educators, retailers, restaurants, and food and beverage manufacturers, and a combination of top-down corporate and government interventions and bottom-up community-based ones. 1198CE71, 399613No single solution creates sufficient impact to reverse obesityNo single solution creates sufficient impact to reverse obesity: only a comprehensive, systemic program of multiple interventions is likely to be effective. 1198CE71, 399614Many interventions are highly cost-effectiveAlmost all of the interventions we analyzed are highly cost-effective from the viewpoint of society.1198CE71, 399615Education and personal responsibility are necessary but not sufficientEducation and encouraging personal responsibility are necessary but not sufficient.1198CE71, 399617Experiment with multiple interventionsSociety should be prepared to experiment with possible interventions. In many intervention areas, impact data from high-quality, randomized control trials are not possible to gather. So, rather than waiting for such data, the relevant sectors of society should be pragmatic with a bias toward action, especially where the risks of intervening are low, using trial and error to flesh out their understanding of potential solutions. 565CA4D9, 399715Types of weight-management services565CA4D9, 399887Causes of obesityUnderstanding the causes of obesity is critical to the success of prevention and treatment strategies. However, while (simply put) obesity occurs when energy intake from food and drink consumption is greater than energy expenditure through the body’s metabolism and physical activity over a prolonged period (resulting in the accumulation of excess body fat), in reality many complex behavioural and societal factors contribute systemically to the current crisis and no single influence dominates.555CD992, 399932Paucity of investment in intervention measuresThe UK invests less than $1 billion a year in prevention activities such as weight-management programs and public health campaigns – i.e. around 1% of the social cost of obesity in the UK. More investment is required.555CD992, 399973A potentially unsustainable financial burden on the health systemThe range of obesity's impacts makes accurate economic analysis challenging; however, a November 2014 study from the McKinsey Global Institute placed the annual economic impact on the UK at around $73bn (£46bn). Earlier analysis and modelling for the 2007 Foresight Report suggested a cost to the NHS of around £4.2bn annually to treat people with health problems related to elevated BMI and a total wider cost to the economy of around £15.8bn (rising to £27bn by 2015 and £49.9bn by 2050).57DE7179, 400018Lost productivityObesity has as a serious impact on UK economic development – constraining economic productivity and increasing business costs – affecting individuals’ ability to get and hold down work, their self-esteem and their underlying mental health.57DE7179, 400018Lost productivityObesity has as a serious impact on UK economic development – constraining economic productivity and increasing business costs – affecting individuals’ ability to get and hold down work, their self-esteem and their underlying mental health.57DE7179, 400061Current incentives are mis-aligned118FF4888, 400083Government obesity efforts are too fragmented to be effectiveGovernment efforts to tackle the obesity issue seem too fragmented to be effective. In the United Kingdom, 15 central government departments; all local authorities with responsibility for health, education, and local planning; 16 EU directorates-general; and a wide range of nongovernmental organizations all have a significant impact on the major intervention areas.118FF4888, 400084Desire to priortise options becomes a barrier to actionA search for the “best” interventions or a single solution could delay action and displace responsibility. Given the seriousness of the obesity issue, the aim should be to do as much as possible as soon as possible.118FF4888 URL:
| | Extrait - Obesity is a complex, systemic, multi-causal problem, rooted in the sedentary nature of modern post-industrial life, more widely available and more affordable food, a change in the nature and mix of diets, psychological stimuli such as stress and epigenetic triggers, and potentially even physiological disruption to the gut microbiome. There is considerable ongoing academic research into the scale and causes of the rapidly rising obesity epidemic. Researchers are digging deep into specific questions and analyzing potential solutions. However, there is a lack of integrated analysis of the holistic program that would be needed to reverse rising obesity, and what it would take to start to deliver such a program.
This discussion paper seeks to start to close this gap. We set out to learn as much as possible from existing research and build on it with our own understanding of micro- and behavioral economics, and McKinsey’s experience and research across sectors, including consumer-facing, public, and health-care sectors. Our aim then has been to step back and attempt to develop a perspective on what might be the building blocks of a societal response that could overcome rising obesity.
|
Link[7] The Role of Business in Multisector Obesity Solutions: Working Together for Positive Change - Workshop in Brief
En citant: Leslie Pray, Roundtable on Obesity Solutions, Food and Nutrition Board, Health and Medicine Division; National Academies of Sciences, Engineering, and Medicine
Publication date: 29 June 2016
Cité par: David Price 3:07 PM 29 June 2016 GMT
URL:
| | Extrait - On April 12, 2016, the Roundtable on Obesity Solutions convened a 1-day workshop in Washington, DC, to examine the role of the business sector in obesity solutions.
The goal of the workshop was threefold:
(1) explore why companies should be involved in obesity solutions and how to encourage them to do so;
(2) identify reasons why businesses might be interested in being involved in obesity solutions;
(3) identify ways in which business can be engaged in obesity solutions.
Nico Pronk, vice president for health management and chief science officer at Health Partners Inc., started the workshop and referred to statistics that show the rapid growth in obesity prevalence among U.S. workers, from 15 to 30 percent over the past three decades. Pronk listed several ways that obesity in the workforce impacts both companies and individuals.
He emphasized the bidirectional connection between healthy companies and thriving communities and put obesity into the context of the social determinants of health model, which predicts that only 20 percent of an individual’s health is related to what happens in the doctor’s office and the remainder to social and economic factors, behaviors, and the physical environment.
He raised four questions for workshop participants to consider:
(1) How can business be engaged?
(2) How does business relate to other sectors in ways that may align efforts?
(3) What are examples of partnerships between businesses and other community stakeholders?
(4) What are opportunities and barriers to engaging business?
This Workshop in Brief highlights key points made during the presentations and discussions and is not intended to provide a comprehensive summary of information shared during the workshop. |
|
|