|
![]()
| Align the school curriculum with obesity, nutrition and activity goals How1 #366479
| The Cochrane Review [4] concluded: We found strong evidence to support beneficial effects of child obesity prevention programmes on BMI, particularly for programmes targeted to children aged six to 12 years. However, given the unexplained heterogeneity and the likelihood of small study bias, these findings must be interpreted cautiously. A broad range of programme components were used in these studies and whilst it is not possible to distinguish which of these components contributed most to the beneficial effects observed, our synthesis indicates the following to be promising policies and strategies: · school curriculum that includes healthy eating, physical activity and body image · increased sessions for physical activity and the development of fundamental movement skills throughout the school week
· improvements in nutritional quality of the food supply in schools
· environments and cultural practices that support children eating healthier foods and being active throughout each day
· support for teachers and other staff to implement health promotion strategies and activities (e.g. professional development, capacity building activities)
· parent support and home activities that encourage children to be more active, eat more nutritious foods and spend less time in screen based activities However, study and evaluation designs need to be strengthened, and reporting extended to capture process and implementation factors, outcomes in relation to measures of equity, longer term outcomes, potential harms and costs.
Childhood obesity prevention research must now move towards identifying how effective intervention components can be embedded within health, education and care systems and achieve long term sustainable impacts. Cost-effective interventions to reduce obesity in the UK 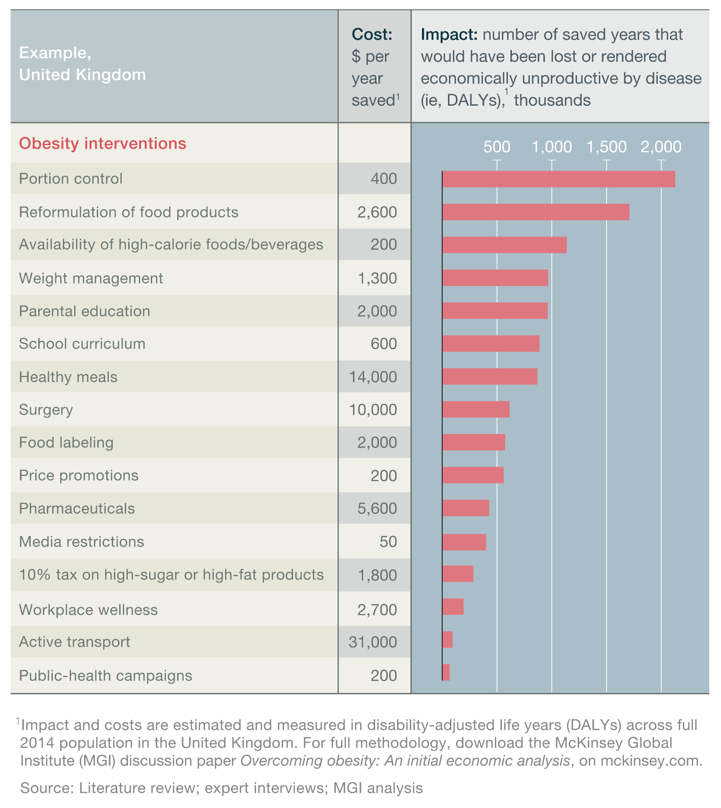
|
+Citations (4) - CitationsAdd new citationList by: CiterankMapLink[1] Overcoming obesity: An initial economic analysis
Author: Richard Dobbs, Corinne Sawers, Fraser Thompson, James Manyika - Jonathan Woetzel, Peter Child, Sorcha McKenna, Angela Spatharou (McKinsey Global Institute)
Publication info: 2014 November
Cited by: David Price 10:20 PM 27 December 2014 GMT
Citerank: (60) 340964Tackling obesity in the UKWith concern growing that the Foresight analysis—that 50% of the UK population could be obese by 2050, at an annual cost to the nation of around £50 billion per year [2]—substantially underestimates the scale of the unfolding obesity crisis, the College of Contemporary Health is working with the wider policy community to develop a whole systems map of the obesity crisis and the potential responses.7F1CEB7, 348675Adopt a whole systems approach to obesityTackling obesity effectively—accomplishing a population wide-shift—requires a comprehensive and integrated whole systems approach, involving a range of measures focusing on individuals, social and other systems, including at the local and community level, and on the interrelated physical, physiological, social and cognitive factors that determine health outcomes.565CA4D9, 348767A potentially unsustainable financial burden on the health systemThe range of obesity's impacts makes accurate economic analysis challenging; however, a November 2014 study from the McKinsey Global Institute placed the annual economic impact on the UK at around $73bn (£46bn). Earlier analysis and modelling for the 2007 Foresight Report suggested a cost to the NHS of around £4.2bn annually to treat people with health problems related to elevated BMI and a total wider cost to the economy of around £15.8bn (rising to £27bn by 2015 and £49.9bn by 2050).57DE7179, 348770Tackling obesityMany policy interventions have been suggested to address the obesity crisis across multiple studies—and indeed many such measures have been implemented, and are being implemented, now. There's recognition too that these interventions need to be part of a coherent and comprehensive whole systems strategy [4]; with some grounds for optimism that such an approach has the potential to accomplish a significant reduction in the prevalence of obesity in the UK across the next decade. [2]565CA4D9, 348780Causes of obesityUnderstanding the causes of obesity is critical to the success of prevention and treatment strategies. However, while (simply put) obesity occurs when energy intake from food and drink consumption is greater than energy expenditure through the body’s metabolism and physical activity over a prolonged period (resulting in the accumulation of excess body fat), in reality many complex behavioural and societal factors contribute systemically to the current crisis and no single influence dominates.555CD992, 352311Lost productivityObesity has as a serious impact on UK economic development – constraining economic productivity and increasing business costs – affecting individuals’ ability to get and hold down work, their self-esteem and their underlying mental health.57DE7179, 352311Lost productivityObesity has as a serious impact on UK economic development – constraining economic productivity and increasing business costs – affecting individuals’ ability to get and hold down work, their self-esteem and their underlying mental health.57DE7179, 352373Invest in weight management servicesThe departments of health in the four nations should extend and increase the provision of weight management services across the country, to mirror the provision of smoking cessation services.565CA4D9, 352710Develop better pharmaceutical obesity therapiesObesity drug sales are forecast to $3.8bn globally in 2018 [2]—in comparison to $57bn for Diabetes drug sales[2]—with evidence suggesting that the modest average weight losses achieved with current anti-obesity agents may be of some clinical benefit [5]. However, the current generation of drugs, which act on the central nervous system to suppress appetite, have raised significant health concerns—including psychiatric disorders, such as suicidal behaviour, depression, and cardiovascular problems.565CA4D9, 352718Invest in employee health and wellbeingEncourage organisations to invest employee health and wellbeing; including a health risk assessment and the provision of resources to help employees address the factors that pose the greatest risk to their health and wellness. [1], [2], [3], [4], [5]565CA4D9, 366161McKinsey Global InstituteThe MGI discussion paper, Overcoming obesity: An initial economic analysis studied studied 74 interventions (in 18 areas) that are being discussed or piloted somewhere around the world to address obesity, including subsidized school meals for all, calorie and nutrition labeling, restrictions on advertising high-calorie food and drinks, and public-health campaigns – with sufficient data found on 44 of the interventions in 16 areas. 58D3ABAB, 366169Obesity Interventions identified by MGI74 interventions – across 18 groups – to reduce obesity.565CA4D9, 366449Deploy and integrate as many interventions as possible at scaleCommission and deploy as many interventions as possible at scale and delivered effectively, and integrated way, by the full range of sectors in society.565CA4D9, 366450Understand how to align incentives and build cooperation109FDEF6, 366452No single solution creates sufficient impact to reverse obesityNo single solution creates sufficient impact to reverse obesity: only a comprehensive, systemic program of multiple interventions is likely to be effective. 1198CE71, 366453Many interventions are highly cost-effectiveAlmost all of the interventions we analyzed are highly cost-effective from the viewpoint of society.1198CE71, 366454Education and personal responsibility are necessary but not sufficientEducation and encouraging personal responsibility are necessary but not sufficient.1198CE71, 366456Co-ordinated multi-party actions are required to tackle obesityCapturing the full potential impact is likely to require commitment from government, employers, educators, retailers, restaurants, and food and beverage manufacturers, and a combination of top-down corporate and government interventions and bottom-up community-based ones. 1198CE71, 366457Government obesity efforts are too fragmented to be effectiveGovernment efforts to tackle the obesity issue seem too fragmented to be effective. In the United Kingdom, 15 central government departments; all local authorities with responsibility for health, education, and local planning; 16 EU directorates-general; and a wide range of nongovernmental organizations all have a significant impact on the major intervention areas. [1]118FF4888, 366458Current incentives are mis-aligned118FF4888, 366460Desire to prioritise options becomes a barrier to actionA search for the “best” interventions or a single solution could delay action and displace responsibility. Given the seriousness of the obesity issue, the aim should be to do as much as possible as soon as possible. [1]118FF4888, 366462Experiment with multiple interventionsSociety should be prepared to experiment with possible interventions. In many intervention areas, impact data from high-quality, randomized control trials are not possible to gather. So, rather than waiting for such data, the relevant sectors of society should be pragmatic with a bias toward action, especially where the risks of intervening are low, using trial and error to flesh out their understanding of potential solutions. 565CA4D9, 366463Paucity of investment in intervention measuresThe UK invests less than $1 billion a year in prevention activities such as weight-management programs and public health campaigns – i.e. around 1% of the social cost of obesity in the UK. More investment is required.555CD992, 366467Encourage active transport (walking and cycling)Government authorities redesign urban planning to facilitate and encourage walking and cycling.565CA4D9, 366479Align the school curriculum with obesity, nutrition and activity goals565CA4D9, 366481Improve surgical interventions for obesity565CA4D9, 366483Types of weight-management services565CA4D9, 366555Employers offer team challenge incentive schemes in the workplaceEmployers provide team challenge activities to encourage physical activity and improved key health indicators in the workplace.565CA4D9, 366557Employers give employees financial incentives to improve healthEmployers provide material incentives to individuals for improved key health indicators (e.g., discounts on insurance premiums, gym membership, prizes).565CA4D9, 366827Develop a coherent fiscal, regulatory and governance frameworkTake every opportunity, iteratively over time, to bring the public fiscal, regulatory and governance framework into alignment with public health goals on obesity. Use taxes, subsidies, targets and pricing signals to incentivise change in behaviour, supply and consumption by aligning measures with the health properties of food and drink and behaviour—and seek, wherever practical, to amplify positive patterns that are aligned with the policy goals and damp those that pull against.565CA4D9, 371556Many obesity policy measures appear to be cost-effective for societyThe recent MGI study [1] reported that almost all of the obesity policy interventions included in its economic analysis appeared to be highly cost-effective at the societal level—i.e. the health-care costs and productivity savings that accrue from reducing obesity through a specific intervention outweighed the direct investment required to deliver that intervention when assessed over the full lifetime of the target population.1198CE71, 399546Tackling obesityMany policy interventions have been suggested to address the obesity crisis across multiple studies—and indeed many such measures have been implemented, and are being implemented, now. There's recognition too that these interventions need to be part of a coherent and comprehensive whole systems strategy [4]; with some grounds for optimism that such an approach has the potential to accomplish a significant reduction in the prevalence of obesity in the UK across the next decade. [2]565CA4D9, 399547Adopt a whole systems approach to obesityTackling obesity effectively—accomplishing a population wide-shift—requires a comprehensive and integrated whole systems approach, involving a range of measures focusing on individuals, social and other systems, including at the local and community level, and on the interrelated physical, physiological, social and cognitive factors that determine health outcomes.565CA4D9, 399548Invest in employee health and wellbeingEncourage organisations to invest employee health and wellbeing; including a health risk assessment and the provision of resources to help employees address the factors that pose the greatest risk to their health and wellness. [1], [2], [3], [4], [5]565CA4D9, 399552Develop a coherent fiscal, regulatory and governance frameworkTake every opportunity, iteratively over time, to bring the public fiscal, regulatory and governance framework into alignment with public health goals on obesity. Use taxes, subsidies, targets and pricing signals to incentivise change in behaviour, supply and consumption by aligning measures with the health properties of food and drink and behaviour—and seek, wherever practical, to amplify positive patterns that are aligned with the policy goals and damp those that pull against.565CA4D9, 399555Many obesity policy measures appear to be cost-effective for societyThe recent MGI study [1] reported that almost all of the obesity policy interventions included in its economic analysis appeared to be highly cost-effective at the societal level—i.e. the health-care costs and productivity savings that accrue from reducing obesity through a specific intervention outweighed the direct investment required to deliver that intervention when assessed over the full lifetime of the target population.1198CE71, 399561Deploy and integrate as many interventions as possible at scaleCommission and deploy as many interventions as possible at scale and delivered effectively, and integrated way, by the full range of sectors in society.565CA4D9, 399567Employers offer team challenge incentive schemes in the workplaceEmployers provide team challenge activities to encourage physical activity and improved key health indicators in the workplace.565CA4D9, 399568Employers give employees financial incentives to improve healthEmployers provide material incentives to individuals for improved key health indicators (e.g., discounts on insurance premiums, gym membership, prizes).565CA4D9, 399575Align the school curriculum with obesity, nutrition and activity goals565CA4D9, 399575Align the school curriculum with obesity, nutrition and activity goals565CA4D9, 399586Develop better pharmaceutical obesity therapiesObesity drug sales are forecast to $3.8bn globally in 2018 [2]—in comparison to $57bn for Diabetes drug sales[2]—with evidence suggesting that the modest average weight losses achieved with current anti-obesity agents may be of some clinical benefit [5]. However, the current generation of drugs, which act on the central nervous system to suppress appetite, have raised significant health concerns—including psychiatric disorders, such as suicidal behaviour, depression, and cardiovascular problems.565CA4D9, 399588Improve surgical interventions for obesity565CA4D9, 399592Invest in weight management servicesThe departments of health in the four nations should extend and increase the provision of weight management services across the country, to mirror the provision of smoking cessation services.565CA4D9, 399599Encourage active transport (walking and cycling)Government authorities redesign urban planning to facilitate and encourage walking and cycling.565CA4D9, 399611Understand how to align incentives and build cooperation109FDEF6, 399612Co-ordinated multi-party actions are required to tackle obesityCapturing the full potential impact is likely to require commitment from government, employers, educators, retailers, restaurants, and food and beverage manufacturers, and a combination of top-down corporate and government interventions and bottom-up community-based ones. 1198CE71, 399613No single solution creates sufficient impact to reverse obesityNo single solution creates sufficient impact to reverse obesity: only a comprehensive, systemic program of multiple interventions is likely to be effective. 1198CE71, 399614Many interventions are highly cost-effectiveAlmost all of the interventions we analyzed are highly cost-effective from the viewpoint of society.1198CE71, 399615Education and personal responsibility are necessary but not sufficientEducation and encouraging personal responsibility are necessary but not sufficient.1198CE71, 399617Experiment with multiple interventionsSociety should be prepared to experiment with possible interventions. In many intervention areas, impact data from high-quality, randomized control trials are not possible to gather. So, rather than waiting for such data, the relevant sectors of society should be pragmatic with a bias toward action, especially where the risks of intervening are low, using trial and error to flesh out their understanding of potential solutions. 565CA4D9, 399715Types of weight-management services565CA4D9, 399887Causes of obesityUnderstanding the causes of obesity is critical to the success of prevention and treatment strategies. However, while (simply put) obesity occurs when energy intake from food and drink consumption is greater than energy expenditure through the body’s metabolism and physical activity over a prolonged period (resulting in the accumulation of excess body fat), in reality many complex behavioural and societal factors contribute systemically to the current crisis and no single influence dominates.555CD992, 399932Paucity of investment in intervention measuresThe UK invests less than $1 billion a year in prevention activities such as weight-management programs and public health campaigns – i.e. around 1% of the social cost of obesity in the UK. More investment is required.555CD992, 399973A potentially unsustainable financial burden on the health systemThe range of obesity's impacts makes accurate economic analysis challenging; however, a November 2014 study from the McKinsey Global Institute placed the annual economic impact on the UK at around $73bn (£46bn). Earlier analysis and modelling for the 2007 Foresight Report suggested a cost to the NHS of around £4.2bn annually to treat people with health problems related to elevated BMI and a total wider cost to the economy of around £15.8bn (rising to £27bn by 2015 and £49.9bn by 2050).57DE7179, 400018Lost productivityObesity has as a serious impact on UK economic development – constraining economic productivity and increasing business costs – affecting individuals’ ability to get and hold down work, their self-esteem and their underlying mental health.57DE7179, 400018Lost productivityObesity has as a serious impact on UK economic development – constraining economic productivity and increasing business costs – affecting individuals’ ability to get and hold down work, their self-esteem and their underlying mental health.57DE7179, 400061Current incentives are mis-aligned118FF4888, 400083Government obesity efforts are too fragmented to be effectiveGovernment efforts to tackle the obesity issue seem too fragmented to be effective. In the United Kingdom, 15 central government departments; all local authorities with responsibility for health, education, and local planning; 16 EU directorates-general; and a wide range of nongovernmental organizations all have a significant impact on the major intervention areas.118FF4888, 400084Desire to priortise options becomes a barrier to actionA search for the “best” interventions or a single solution could delay action and displace responsibility. Given the seriousness of the obesity issue, the aim should be to do as much as possible as soon as possible.118FF4888 URL:
|
Link[2] Adoption of obesity prevention policies and practices by Australian primary schools: 2006 to 2013
Author: N. Nathan, L. Wolfenden, C. M.Williams, S. L. Yoong, C. Lecathelinais - A.C.Bell, R. Wyse, R. Sutherland, J. Wiggers
Publication info: 2014 December, 16, Health Educ Res. 2014 Dec 16. pii: cyu068
Cited by: David Price 10:23 PM 27 December 2014 GMT
Citerank: (1) 399575Align the school curriculum with obesity, nutrition and activity goals565CA4D9
URL: | | Excerpt / Summary Despite significant investment in many countries, the extent of schools' adoption of obesity prevention policies and practices has not been widely reported. The aims of this article are to describe Australian schools' adoption of healthy eating and physical activity policies and practices over an 8-year period and to determine if their adoption varies according to schools' size, geographic or socio-economic location. Between 2006 and 2013, a representative randomly selected cohort of primary schools (n = 476) in New South Wales, Australia, participated in four telephone interviews. Repeated measures logistic regression analyses using a Generalised Estimating Equation (GEE) framework were undertaken to assess change over time. The prevalence of all four of the healthy eating practices and one physical activity practice significantly increased, while the prevalence of one physical activity practice significantly decreased. The adoption of practices did not differ by school characteristics. Government investment can equitably enhance school adoption of some obesity prevention policies and practices on a jurisdiction-wide basis. Additional and/or different implementation strategies may be required to facilitate greater adoption of physical activity practices. Ongoing monitoring of school adoption of school policies and practices is needed to ensure the intended benefits of government investment are achieved. |
Link[3] Overcoming obesity: An initial economic analysis
Author: Richard Dobbs, Corinne Sawers, Fraser Thompson, James Manyika - Jonathan Woetzel, Peter Child, Sorcha McKenna, Angela Spatharou (McKinsey Global Institute)
Publication info: 2014 November
Cited by: David Price 8:26 PM 5 January 2015 GMT
Citerank: (60) 340964Tackling obesity in the UKWith concern growing that the Foresight analysis—that 50% of the UK population could be obese by 2050, at an annual cost to the nation of around £50 billion per year [2]—substantially underestimates the scale of the unfolding obesity crisis, the College of Contemporary Health is working with the wider policy community to develop a whole systems map of the obesity crisis and the potential responses.7F1CEB7, 348675Adopt a whole systems approach to obesityTackling obesity effectively—accomplishing a population wide-shift—requires a comprehensive and integrated whole systems approach, involving a range of measures focusing on individuals, social and other systems, including at the local and community level, and on the interrelated physical, physiological, social and cognitive factors that determine health outcomes.565CA4D9, 348767A potentially unsustainable financial burden on the health systemThe range of obesity's impacts makes accurate economic analysis challenging; however, a November 2014 study from the McKinsey Global Institute placed the annual economic impact on the UK at around $73bn (£46bn). Earlier analysis and modelling for the 2007 Foresight Report suggested a cost to the NHS of around £4.2bn annually to treat people with health problems related to elevated BMI and a total wider cost to the economy of around £15.8bn (rising to £27bn by 2015 and £49.9bn by 2050).57DE7179, 348770Tackling obesityMany policy interventions have been suggested to address the obesity crisis across multiple studies—and indeed many such measures have been implemented, and are being implemented, now. There's recognition too that these interventions need to be part of a coherent and comprehensive whole systems strategy [4]; with some grounds for optimism that such an approach has the potential to accomplish a significant reduction in the prevalence of obesity in the UK across the next decade. [2]565CA4D9, 348780Causes of obesityUnderstanding the causes of obesity is critical to the success of prevention and treatment strategies. However, while (simply put) obesity occurs when energy intake from food and drink consumption is greater than energy expenditure through the body’s metabolism and physical activity over a prolonged period (resulting in the accumulation of excess body fat), in reality many complex behavioural and societal factors contribute systemically to the current crisis and no single influence dominates.555CD992, 352311Lost productivityObesity has as a serious impact on UK economic development – constraining economic productivity and increasing business costs – affecting individuals’ ability to get and hold down work, their self-esteem and their underlying mental health.57DE7179, 352311Lost productivityObesity has as a serious impact on UK economic development – constraining economic productivity and increasing business costs – affecting individuals’ ability to get and hold down work, their self-esteem and their underlying mental health.57DE7179, 352373Invest in weight management servicesThe departments of health in the four nations should extend and increase the provision of weight management services across the country, to mirror the provision of smoking cessation services.565CA4D9, 352710Develop better pharmaceutical obesity therapiesObesity drug sales are forecast to $3.8bn globally in 2018 [2]—in comparison to $57bn for Diabetes drug sales[2]—with evidence suggesting that the modest average weight losses achieved with current anti-obesity agents may be of some clinical benefit [5]. However, the current generation of drugs, which act on the central nervous system to suppress appetite, have raised significant health concerns—including psychiatric disorders, such as suicidal behaviour, depression, and cardiovascular problems.565CA4D9, 352718Invest in employee health and wellbeingEncourage organisations to invest employee health and wellbeing; including a health risk assessment and the provision of resources to help employees address the factors that pose the greatest risk to their health and wellness. [1], [2], [3], [4], [5]565CA4D9, 366161McKinsey Global InstituteThe MGI discussion paper, Overcoming obesity: An initial economic analysis studied studied 74 interventions (in 18 areas) that are being discussed or piloted somewhere around the world to address obesity, including subsidized school meals for all, calorie and nutrition labeling, restrictions on advertising high-calorie food and drinks, and public-health campaigns – with sufficient data found on 44 of the interventions in 16 areas. 58D3ABAB, 366169Obesity Interventions identified by MGI74 interventions – across 18 groups – to reduce obesity.565CA4D9, 366449Deploy and integrate as many interventions as possible at scaleCommission and deploy as many interventions as possible at scale and delivered effectively, and integrated way, by the full range of sectors in society.565CA4D9, 366450Understand how to align incentives and build cooperation109FDEF6, 366452No single solution creates sufficient impact to reverse obesityNo single solution creates sufficient impact to reverse obesity: only a comprehensive, systemic program of multiple interventions is likely to be effective. 1198CE71, 366453Many interventions are highly cost-effectiveAlmost all of the interventions we analyzed are highly cost-effective from the viewpoint of society.1198CE71, 366454Education and personal responsibility are necessary but not sufficientEducation and encouraging personal responsibility are necessary but not sufficient.1198CE71, 366456Co-ordinated multi-party actions are required to tackle obesityCapturing the full potential impact is likely to require commitment from government, employers, educators, retailers, restaurants, and food and beverage manufacturers, and a combination of top-down corporate and government interventions and bottom-up community-based ones. 1198CE71, 366457Government obesity efforts are too fragmented to be effectiveGovernment efforts to tackle the obesity issue seem too fragmented to be effective. In the United Kingdom, 15 central government departments; all local authorities with responsibility for health, education, and local planning; 16 EU directorates-general; and a wide range of nongovernmental organizations all have a significant impact on the major intervention areas. [1]118FF4888, 366458Current incentives are mis-aligned118FF4888, 366460Desire to prioritise options becomes a barrier to actionA search for the “best” interventions or a single solution could delay action and displace responsibility. Given the seriousness of the obesity issue, the aim should be to do as much as possible as soon as possible. [1]118FF4888, 366462Experiment with multiple interventionsSociety should be prepared to experiment with possible interventions. In many intervention areas, impact data from high-quality, randomized control trials are not possible to gather. So, rather than waiting for such data, the relevant sectors of society should be pragmatic with a bias toward action, especially where the risks of intervening are low, using trial and error to flesh out their understanding of potential solutions. 565CA4D9, 366463Paucity of investment in intervention measuresThe UK invests less than $1 billion a year in prevention activities such as weight-management programs and public health campaigns – i.e. around 1% of the social cost of obesity in the UK. More investment is required.555CD992, 366467Encourage active transport (walking and cycling)Government authorities redesign urban planning to facilitate and encourage walking and cycling.565CA4D9, 366479Align the school curriculum with obesity, nutrition and activity goals565CA4D9, 366481Improve surgical interventions for obesity565CA4D9, 366483Types of weight-management services565CA4D9, 366555Employers offer team challenge incentive schemes in the workplaceEmployers provide team challenge activities to encourage physical activity and improved key health indicators in the workplace.565CA4D9, 366557Employers give employees financial incentives to improve healthEmployers provide material incentives to individuals for improved key health indicators (e.g., discounts on insurance premiums, gym membership, prizes).565CA4D9, 366827Develop a coherent fiscal, regulatory and governance frameworkTake every opportunity, iteratively over time, to bring the public fiscal, regulatory and governance framework into alignment with public health goals on obesity. Use taxes, subsidies, targets and pricing signals to incentivise change in behaviour, supply and consumption by aligning measures with the health properties of food and drink and behaviour—and seek, wherever practical, to amplify positive patterns that are aligned with the policy goals and damp those that pull against.565CA4D9, 371556Many obesity policy measures appear to be cost-effective for societyThe recent MGI study [1] reported that almost all of the obesity policy interventions included in its economic analysis appeared to be highly cost-effective at the societal level—i.e. the health-care costs and productivity savings that accrue from reducing obesity through a specific intervention outweighed the direct investment required to deliver that intervention when assessed over the full lifetime of the target population.1198CE71, 399546Tackling obesityMany policy interventions have been suggested to address the obesity crisis across multiple studies—and indeed many such measures have been implemented, and are being implemented, now. There's recognition too that these interventions need to be part of a coherent and comprehensive whole systems strategy [4]; with some grounds for optimism that such an approach has the potential to accomplish a significant reduction in the prevalence of obesity in the UK across the next decade. [2]565CA4D9, 399547Adopt a whole systems approach to obesityTackling obesity effectively—accomplishing a population wide-shift—requires a comprehensive and integrated whole systems approach, involving a range of measures focusing on individuals, social and other systems, including at the local and community level, and on the interrelated physical, physiological, social and cognitive factors that determine health outcomes.565CA4D9, 399548Invest in employee health and wellbeingEncourage organisations to invest employee health and wellbeing; including a health risk assessment and the provision of resources to help employees address the factors that pose the greatest risk to their health and wellness. [1], [2], [3], [4], [5]565CA4D9, 399552Develop a coherent fiscal, regulatory and governance frameworkTake every opportunity, iteratively over time, to bring the public fiscal, regulatory and governance framework into alignment with public health goals on obesity. Use taxes, subsidies, targets and pricing signals to incentivise change in behaviour, supply and consumption by aligning measures with the health properties of food and drink and behaviour—and seek, wherever practical, to amplify positive patterns that are aligned with the policy goals and damp those that pull against.565CA4D9, 399555Many obesity policy measures appear to be cost-effective for societyThe recent MGI study [1] reported that almost all of the obesity policy interventions included in its economic analysis appeared to be highly cost-effective at the societal level—i.e. the health-care costs and productivity savings that accrue from reducing obesity through a specific intervention outweighed the direct investment required to deliver that intervention when assessed over the full lifetime of the target population.1198CE71, 399561Deploy and integrate as many interventions as possible at scaleCommission and deploy as many interventions as possible at scale and delivered effectively, and integrated way, by the full range of sectors in society.565CA4D9, 399567Employers offer team challenge incentive schemes in the workplaceEmployers provide team challenge activities to encourage physical activity and improved key health indicators in the workplace.565CA4D9, 399568Employers give employees financial incentives to improve healthEmployers provide material incentives to individuals for improved key health indicators (e.g., discounts on insurance premiums, gym membership, prizes).565CA4D9, 399575Align the school curriculum with obesity, nutrition and activity goals565CA4D9, 399575Align the school curriculum with obesity, nutrition and activity goals565CA4D9, 399586Develop better pharmaceutical obesity therapiesObesity drug sales are forecast to $3.8bn globally in 2018 [2]—in comparison to $57bn for Diabetes drug sales[2]—with evidence suggesting that the modest average weight losses achieved with current anti-obesity agents may be of some clinical benefit [5]. However, the current generation of drugs, which act on the central nervous system to suppress appetite, have raised significant health concerns—including psychiatric disorders, such as suicidal behaviour, depression, and cardiovascular problems.565CA4D9, 399588Improve surgical interventions for obesity565CA4D9, 399592Invest in weight management servicesThe departments of health in the four nations should extend and increase the provision of weight management services across the country, to mirror the provision of smoking cessation services.565CA4D9, 399599Encourage active transport (walking and cycling)Government authorities redesign urban planning to facilitate and encourage walking and cycling.565CA4D9, 399611Understand how to align incentives and build cooperation109FDEF6, 399612Co-ordinated multi-party actions are required to tackle obesityCapturing the full potential impact is likely to require commitment from government, employers, educators, retailers, restaurants, and food and beverage manufacturers, and a combination of top-down corporate and government interventions and bottom-up community-based ones. 1198CE71, 399613No single solution creates sufficient impact to reverse obesityNo single solution creates sufficient impact to reverse obesity: only a comprehensive, systemic program of multiple interventions is likely to be effective. 1198CE71, 399614Many interventions are highly cost-effectiveAlmost all of the interventions we analyzed are highly cost-effective from the viewpoint of society.1198CE71, 399615Education and personal responsibility are necessary but not sufficientEducation and encouraging personal responsibility are necessary but not sufficient.1198CE71, 399617Experiment with multiple interventionsSociety should be prepared to experiment with possible interventions. In many intervention areas, impact data from high-quality, randomized control trials are not possible to gather. So, rather than waiting for such data, the relevant sectors of society should be pragmatic with a bias toward action, especially where the risks of intervening are low, using trial and error to flesh out their understanding of potential solutions. 565CA4D9, 399715Types of weight-management services565CA4D9, 399887Causes of obesityUnderstanding the causes of obesity is critical to the success of prevention and treatment strategies. However, while (simply put) obesity occurs when energy intake from food and drink consumption is greater than energy expenditure through the body’s metabolism and physical activity over a prolonged period (resulting in the accumulation of excess body fat), in reality many complex behavioural and societal factors contribute systemically to the current crisis and no single influence dominates.555CD992, 399932Paucity of investment in intervention measuresThe UK invests less than $1 billion a year in prevention activities such as weight-management programs and public health campaigns – i.e. around 1% of the social cost of obesity in the UK. More investment is required.555CD992, 399973A potentially unsustainable financial burden on the health systemThe range of obesity's impacts makes accurate economic analysis challenging; however, a November 2014 study from the McKinsey Global Institute placed the annual economic impact on the UK at around $73bn (£46bn). Earlier analysis and modelling for the 2007 Foresight Report suggested a cost to the NHS of around £4.2bn annually to treat people with health problems related to elevated BMI and a total wider cost to the economy of around £15.8bn (rising to £27bn by 2015 and £49.9bn by 2050).57DE7179, 400018Lost productivityObesity has as a serious impact on UK economic development – constraining economic productivity and increasing business costs – affecting individuals’ ability to get and hold down work, their self-esteem and their underlying mental health.57DE7179, 400018Lost productivityObesity has as a serious impact on UK economic development – constraining economic productivity and increasing business costs – affecting individuals’ ability to get and hold down work, their self-esteem and their underlying mental health.57DE7179, 400061Current incentives are mis-aligned118FF4888, 400083Government obesity efforts are too fragmented to be effectiveGovernment efforts to tackle the obesity issue seem too fragmented to be effective. In the United Kingdom, 15 central government departments; all local authorities with responsibility for health, education, and local planning; 16 EU directorates-general; and a wide range of nongovernmental organizations all have a significant impact on the major intervention areas.118FF4888, 400084Desire to priortise options becomes a barrier to actionA search for the “best” interventions or a single solution could delay action and displace responsibility. Given the seriousness of the obesity issue, the aim should be to do as much as possible as soon as possible.118FF4888 URL:
|
Link[4] Interventions for preventing obesity in children
Author: E. Waters E, A. de Silva-Sanigorski, B.J. Hall, T. Brown K. J. Campbell - Y. Gao, R. Armstrong R, L. Prosser , C. D. Summerbell
Publication info: 2011
Cited by: David Price 8:30 PM 5 January 2015 GMT
Citerank: (1) 399575Align the school curriculum with obesity, nutrition and activity goals565CA4D9
URL:
| | Excerpt / Summary Childhood obesity can cause social, psychological and health problems, and is linked to obesity later in life and poor health outcomes as an adult. Obesity development is related to physical activity and nutrition. To prevent obesity, 55 studies conducted internationally have looked at programmes aiming to improve either or both of these behaviours. Although many studies were able to improve children’s nutrition or physical activity to some extent, only some studies were able to see an effect of the programme on children’s levels of fatness.
When we combined the studies, we were able to see that these programmes made a positive difference, but there was much variation between the study findings which we could not explain. Also, it appeared that the findings may be biased by missing small studies with negative findings. We also tried to work out why some programmes work better than others, and whether there was potential harm associated with children being involved in the programmes.
Although only a few studies looked at whether programmes were harmful, the results suggest that those obesity prevention strategies do not increase body image concerns, unhealthy dieting practices, level of underweight, or unhealthy attitudes to weight, and that all children can benefit. It is important that more studies in very young children and adolescents are conducted to find out more about obesity prevention in these age groups, and also that we assess how long the intervention effects last. Also, we need to develop ways of ensuring that research findings benefit all children by embedding the successful programme activities into everyday practices in homes, schools, child care settings, the health system and the wider community. |
|
|