|
![]()
| A profound impact on the health of the population What1 #348776 Obesity is responsible for more than 9,000 premature deaths each year in England, reduces life expectancy on average by nine years, and is a major risk factor in wide range of serious health problems including Type 2 diabetes (5 x), cancer (3 x the risk of colon cancer), and heart disease (2.5 x). | 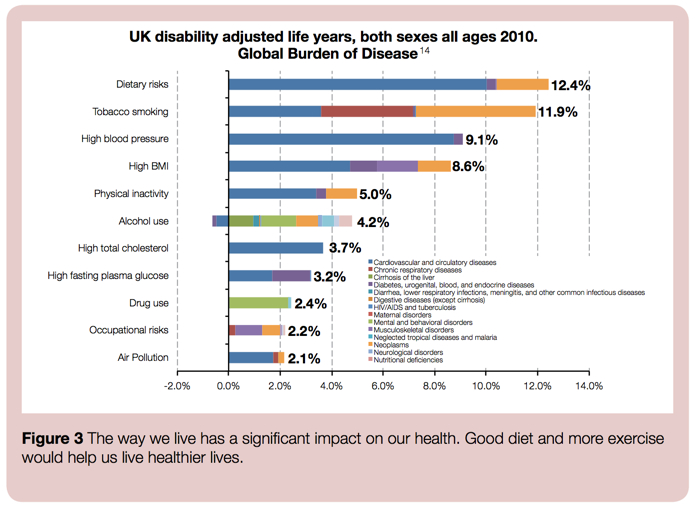
Source: Public Health England [9] Compared with a non-obese man, an obese man is: - five times more likely to develop type 2 diabetes
- three times more likely to develop cancer of the colon
- more than two and a half times more likely to develop high blood pressure – a major risk factor for stroke and heart disease.
An obese woman, compared with a non-obese woman, is: - almost thirteen times more likely to develop type 2 diabetes
- more than four times more likely to develop high blood pressure
- more than three times more likely to have a heart attack.
Risks of other diseases, including angina, gall bladder disease, liver disease, ovarian cancer, osteoarthritis and stroke, are also increased. If current trends persist, one in three people will be obese by 2034 and one in ten will develop type II diabetes (Figure 9, below); whereas, reducing obesity back to 1993 levels, would avoid five million cases of disease (Figure 10, below). 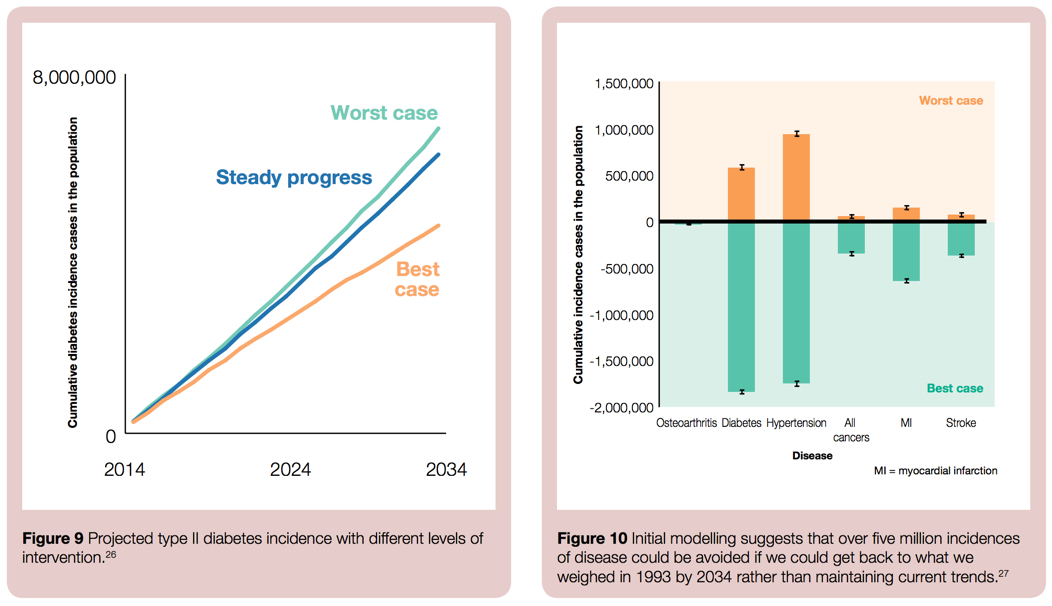
Source: Public Health England [9] - Around 58% of type 2 diabetes, 21% of heart disease and between 8% and 42% of certain cancers (endometrial, breast, and colon) are attributable to excess body fat.
- Obesity reduces life expectancy by an average 9 years and is responsible for 9,000 premature deaths a year in England.
- In addition, people who are obese can experience stigmatisation and bullying, which can lead to depression and low self-esteem. [1]
|
+Citations (9) - CitationsAdd new citationList by: CiterankMapLink[1] Foresight Report - Reducing obesity: future choices
Author: Bryony Butland et al. - Government Office for Science
Publication info: 2007 October, 17
Cited by: David Price 9:13 AM 28 July 2014 GMT
Citerank: (28) 340964Tackling obesity in the UKWith concern growing that the Foresight analysis—that 50% of the UK population could be obese by 2050, at an annual cost to the nation of around £50 billion per year [2]—substantially underestimates the scale of the unfolding obesity crisis, the College of Contemporary Health is working with the wider policy community to develop a whole systems map of the obesity crisis and the potential responses.7F1CEB7, 348675Adopt a whole systems approach to obesityTackling obesity effectively—accomplishing a population wide-shift—requires a comprehensive and integrated whole systems approach, involving a range of measures focusing on individuals, social and other systems, including at the local and community level, and on the interrelated physical, physiological, social and cognitive factors that determine health outcomes.565CA4D9, 348688Impacts of obesityObesity presents a significant threat to the health of the UK population and a significant drain on the nation's financial resources. 24.9% of adults in England are obese—with a body mass index of over 30—62% of adults are either overweight or obese (with a BMI of over 25), and 32% of 10–11-year-olds are overweight or obese. The annual cost of obesity to the UK is estimated to be £27bn–£46bn [1], [2]; although international comparisons suggest that the true cost could be significantly higher.57DE7179, 348693Stakeholders – Groups & ActionsExplore the map via the different stakeholder groups and the measures each group can take to help tackle the obesity crisis.58D3ABAB, 348767A potentially unsustainable financial burden on the health systemThe range of obesity's impacts makes accurate economic analysis challenging; however, a November 2014 study from the McKinsey Global Institute placed the annual economic impact on the UK at around $73bn (£46bn). Earlier analysis and modelling for the 2007 Foresight Report suggested a cost to the NHS of around £4.2bn annually to treat people with health problems related to elevated BMI and a total wider cost to the economy of around £15.8bn (rising to £27bn by 2015 and £49.9bn by 2050).57DE7179, 348770Tackling obesityMany policy interventions have been suggested to address the obesity crisis across multiple studies—and indeed many such measures have been implemented, and are being implemented, now. There's recognition too that these interventions need to be part of a coherent and comprehensive whole systems strategy [4]; with some grounds for optimism that such an approach has the potential to accomplish a significant reduction in the prevalence of obesity in the UK across the next decade. [2]565CA4D9, 348775Modelling suggests the majority of UK population may be obese by 2050The prevalence of obesity in the UK more than doubled in the 25 years to 2007. In England, nearly a quarter of adults and about 10% of children were obese in 2007, with a further 20–25% of children overweight. The Foresight report extrapolated that 40% of Britons might be being obese by 2025, with Britain being a mainly obese society by 2050.1198CE71, 348779Involve all stakeholders in the process of changeReversing the rising trend and addressing the prospect of the rising health burden and societal costs will be demanding and will necessitate major changes in behaviour – not only in individuals, but also in families, communities, organisations and economic markets.565CA4D9, 348780Causes of obesityUnderstanding the causes of obesity is critical to the success of prevention and treatment strategies. However, while (simply put) obesity occurs when energy intake from food and drink consumption is greater than energy expenditure through the body’s metabolism and physical activity over a prolonged period (resulting in the accumulation of excess body fat), in reality many complex behavioural and societal factors contribute systemically to the current crisis and no single influence dominates.555CD992, 351674Inequality of impactAlthough obesity occurs across all population groups, it impacts disproportionately on the socially and economically disadvantaged and some ethnic minorities. [8]57DE7179, 352390Industrial way of life is obesogenicRapid societal changes—for example, in food production, motorised transport and work/home lifestyle patterns—have placed human physiology (which has evolved to cope with an under-supply of food and high energy expenditure) under new stresses, and revealed an underlying genetic tendency to accumulate and conserve energy (i.e. gain weight) in a high proportion of the population. In this sense, obesity can be construed as a normal physiological response to an abnormal environment.555CD992, 352390Industrial way of life is obesogenicRapid societal changes—for example, in food production, motorised transport and work/home lifestyle patterns—have placed human physiology (which has evolved to cope with an under-supply of food and high energy expenditure) under new stresses, and revealed an underlying genetic tendency to accumulate and conserve energy (i.e. gain weight) in a high proportion of the population. In this sense, obesity can be construed as a normal physiological response to an abnormal environment.555CD992, 365986Foresight – Obesity System MapObesity occurs when energy intake from food and drink consumption is greater than energy expenditure through the body’s metabolism and physical activity over a prolonged period, resulting in the accumulation of excess body fat. However there are many complex behavioural and societal factors that combine to contribute to the causes of obesity.7F1CEB7, 366467Encourage active transport (walking and cycling)Government authorities redesign urban planning to facilitate and encourage walking and cycling.565CA4D9, 366990What costs should be included in the financial analysis?What cost factors should be included in the assessment of the overall financial impact of obesity on the UK economy?8FFB597, 399546Tackling obesityMany policy interventions have been suggested to address the obesity crisis across multiple studies—and indeed many such measures have been implemented, and are being implemented, now. There's recognition too that these interventions need to be part of a coherent and comprehensive whole systems strategy [4]; with some grounds for optimism that such an approach has the potential to accomplish a significant reduction in the prevalence of obesity in the UK across the next decade. [2]565CA4D9, 399547Adopt a whole systems approach to obesityTackling obesity effectively—accomplishing a population wide-shift—requires a comprehensive and integrated whole systems approach, involving a range of measures focusing on individuals, social and other systems, including at the local and community level, and on the interrelated physical, physiological, social and cognitive factors that determine health outcomes.565CA4D9, 399557Involve all stakeholders in the process of changeReversing the rising trend and addressing the prospect of the rising health burden and societal costs will be demanding and will necessitate major changes in behaviour – not only in individuals, but also in families, communities, organisations and economic markets.565CA4D9, 399599Encourage active transport (walking and cycling)Government authorities redesign urban planning to facilitate and encourage walking and cycling.565CA4D9, 399887Causes of obesityUnderstanding the causes of obesity is critical to the success of prevention and treatment strategies. However, while (simply put) obesity occurs when energy intake from food and drink consumption is greater than energy expenditure through the body’s metabolism and physical activity over a prolonged period (resulting in the accumulation of excess body fat), in reality many complex behavioural and societal factors contribute systemically to the current crisis and no single influence dominates.555CD992, 399889Industrial way of life is obesogenicRapid societal changes—for example, in food production, motorised transport and work/home lifestyle patterns—have placed human physiology (which has evolved to cope with an under-supply of food and high energy expenditure) under new stresses, and revealed an underlying genetic tendency to accumulate and conserve energy (i.e. gain weight) in a high proportion of the population. In this sense, obesity can be construed as a normal physiological response to an abnormal environment.555CD992, 399889Industrial way of life is obesogenicRapid societal changes—for example, in food production, motorised transport and work/home lifestyle patterns—have placed human physiology (which has evolved to cope with an under-supply of food and high energy expenditure) under new stresses, and revealed an underlying genetic tendency to accumulate and conserve energy (i.e. gain weight) in a high proportion of the population. In this sense, obesity can be construed as a normal physiological response to an abnormal environment.555CD992, 399972Impacts of obesityObesity presents a significant threat to the health of the UK population and a significant drain on the nation's financial resources. 23% of adults are obese—with a body mass index of over 30—61% of adults are either overweight or obese (with a BMI of over 25), and 33% of 10–11-year-olds are overweight or obese. The annual cost of obesity to the UK economy has been estimated to be £27bn–£46bn [1], [2]; although international comparisons suggest that the true cost could be significantly higher.57DE7179, 399973A potentially unsustainable financial burden on the health systemThe range of obesity's impacts makes accurate economic analysis challenging; however, a November 2014 study from the McKinsey Global Institute placed the annual economic impact on the UK at around $73bn (£46bn). Earlier analysis and modelling for the 2007 Foresight Report suggested a cost to the NHS of around £4.2bn annually to treat people with health problems related to elevated BMI and a total wider cost to the economy of around £15.8bn (rising to £27bn by 2015 and £49.9bn by 2050).57DE7179, 399974A profound impact on the health of the populationObesity is responsible for more than 9,000 premature deaths each year in England, reduces life expectancy on average by nine years, and is a major risk factor in wide range of serious health problems including Type 2 diabetes (5 x), cancer (3 x the risk of colon cancer), and heart disease (2.5 x).57DE7179, 399978Modelling suggests the majority of UK population may be obese by 2050The prevalence of obesity in the UK more than doubled in the 25 years to 2007. In England, nearly a quarter of adults and about 10% of children were obese in 2007, with a further 20–25% of children overweight. The Foresight report extrapolated that 40% of Britons might be being obese by 2025, with Britain being a mainly obese society by 2050.1198CE71, 399980What costs should be included in the financial analysis?What cost factors should be included in the assessment of the overall financial impact of obesity on the UK economy?8FFB597, 399984Inequality of impactAlthough obesity occurs across all population groups, it impacts disproportionately on the socially and economically disadvantaged and some ethnic minorities. [8]57DE7179 URL:
|
Link[2] Healthy Lives, Healthy People: A call to action on obesity in England
Author: Department of Health
Publication info: 2011 October 13
Cited by: David Price 9:38 AM 5 September 2014 GMT
Citerank: (16) 340964Tackling obesity in the UKWith concern growing that the Foresight analysis—that 50% of the UK population could be obese by 2050, at an annual cost to the nation of around £50 billion per year [2]—substantially underestimates the scale of the unfolding obesity crisis, the College of Contemporary Health is working with the wider policy community to develop a whole systems map of the obesity crisis and the potential responses.7F1CEB7, 348688Impacts of obesityObesity presents a significant threat to the health of the UK population and a significant drain on the nation's financial resources. 24.9% of adults in England are obese—with a body mass index of over 30—62% of adults are either overweight or obese (with a BMI of over 25), and 32% of 10–11-year-olds are overweight or obese. The annual cost of obesity to the UK is estimated to be £27bn–£46bn [1], [2]; although international comparisons suggest that the true cost could be significantly higher.57DE7179, 348780Causes of obesityUnderstanding the causes of obesity is critical to the success of prevention and treatment strategies. However, while (simply put) obesity occurs when energy intake from food and drink consumption is greater than energy expenditure through the body’s metabolism and physical activity over a prolonged period (resulting in the accumulation of excess body fat), in reality many complex behavioural and societal factors contribute systemically to the current crisis and no single influence dominates.555CD992, 348780Causes of obesityUnderstanding the causes of obesity is critical to the success of prevention and treatment strategies. However, while (simply put) obesity occurs when energy intake from food and drink consumption is greater than energy expenditure through the body’s metabolism and physical activity over a prolonged period (resulting in the accumulation of excess body fat), in reality many complex behavioural and societal factors contribute systemically to the current crisis and no single influence dominates.555CD992, 351719Actions – Local Authorities2794CAE1, 352281Changes required across many different policy areasObesity has to be seen as not just a technical, food, physical activity or healthcare problem but a challenge for what sort of society is being built. Small, incremental, publicity-driven (i.e. social market-based) changes might suit the existing balance of policy interests, but a more extensive, co-ordinated, cross-sectoral action would be more effective.1198CE71, 352311Lost productivityObesity has as a serious impact on UK economic development – constraining economic productivity and increasing business costs – affecting individuals’ ability to get and hold down work, their self-esteem and their underlying mental health.57DE7179, 352312Target interventions across the whole course of lifeTackling obesity effectively requires the adoption of a life course approach – from pre-conception through pregnancy, infancy, early years, childhood, adolescence and teenage years, and through to adulthood and preparing for older age. There are specific opportunities and challenges at each stage of the life course and action is needed at all ages to avert the short- and long-term consequences of excess weight and to ensure that health inequalities are addressed. 565CA4D9, 352314Actions – Central Government2794CAE1, 399558Changes required across many different policy areasObesity has to be seen as not just a technical, food, physical activity or healthcare problem but a challenge for what sort of society is being built. Small, incremental, publicity-driven (i.e. social market-based) changes might suit the existing balance of policy interests, but a more extensive, co-ordinated, cross-sectoral action would be more effective.1198CE71, 399559Target interventions across the whole course of lifeTackling obesity effectively requires the adoption of a life course approach – from pre-conception through pregnancy, infancy, early years, childhood, adolescence and teenage years, and through to adulthood and preparing for older age. There are specific opportunities and challenges at each stage of the life course and action is needed at all ages to avert the short- and long-term consequences of excess weight and to ensure that health inequalities are addressed. 565CA4D9, 399887Causes of obesityUnderstanding the causes of obesity is critical to the success of prevention and treatment strategies. However, while (simply put) obesity occurs when energy intake from food and drink consumption is greater than energy expenditure through the body’s metabolism and physical activity over a prolonged period (resulting in the accumulation of excess body fat), in reality many complex behavioural and societal factors contribute systemically to the current crisis and no single influence dominates.555CD992, 399887Causes of obesityUnderstanding the causes of obesity is critical to the success of prevention and treatment strategies. However, while (simply put) obesity occurs when energy intake from food and drink consumption is greater than energy expenditure through the body’s metabolism and physical activity over a prolonged period (resulting in the accumulation of excess body fat), in reality many complex behavioural and societal factors contribute systemically to the current crisis and no single influence dominates.555CD992, 399972Impacts of obesityObesity presents a significant threat to the health of the UK population and a significant drain on the nation's financial resources. 23% of adults are obese—with a body mass index of over 30—61% of adults are either overweight or obese (with a BMI of over 25), and 33% of 10–11-year-olds are overweight or obese. The annual cost of obesity to the UK economy has been estimated to be £27bn–£46bn [1], [2]; although international comparisons suggest that the true cost could be significantly higher.57DE7179, 399974A profound impact on the health of the populationObesity is responsible for more than 9,000 premature deaths each year in England, reduces life expectancy on average by nine years, and is a major risk factor in wide range of serious health problems including Type 2 diabetes (5 x), cancer (3 x the risk of colon cancer), and heart disease (2.5 x).57DE7179, 400018Lost productivityObesity has as a serious impact on UK economic development – constraining economic productivity and increasing business costs – affecting individuals’ ability to get and hold down work, their self-esteem and their underlying mental health.57DE7179 URL:
|
Link[3] The medical risks of obesity
Author: X. Pi-Sunyer
Publication info: 2009, Postgrad Med. 2009 Nov;121(6):21-33. doi: 10.3810/pgm.2009.11.2074.
Cited by: David Price 5:01 PM 5 September 2014 GMT
Citerank: (1) 399974A profound impact on the health of the populationObesity is responsible for more than 9,000 premature deaths each year in England, reduces life expectancy on average by nine years, and is a major risk factor in wide range of serious health problems including Type 2 diabetes (5 x), cancer (3 x the risk of colon cancer), and heart disease (2.5 x).57DE7179
URL: | | Excerpt / Summary Obesity is a significant risk factor for and contributor to increased morbidity and mortality, most importantly from cardiovascular disease (CVD) and diabetes, but also from cancer and chronic diseases, including osteoarthritis, liver and kidney disease, sleep apnea, and depression. The prevalence of obesity has increased steadily over the past 5 decades, and obesity may have a significant impact on quality-adjusted life years. Obesity is also strongly associated with an increased risk of all-cause mortality as well as cardiovascular and cancer mortality. Despite the substantial effects of obesity, weight loss can result in a significant reduction in risk for the majority of these comorbid conditions. Those comorbidities most closely linked to obesity must be identified to increase awareness of potential adverse outcomes. This will allow health care professionals to identify and implement appropriate interventions to reduce patient risk and mortality. A systematic search strategy was used to identify published literature between 1995 and 2008 that reported data from prospective longitudinal studies of obesity and comorbid medical conditions. This article will review evidence for significant associations of obesity with comorbidities to provide information useful for optimal patient management. |
Link[4] Health risks of adult obesity
Author: Public Health England – Obesity
Cited by: David Price 5:04 PM 5 September 2014 GMT
Citerank: (21) 351181Increased risk of several cancersThe risk of several cancers is higher in obese people, including endometrial, breast and colon cancers. BMI is associated with cancer risk, with substantial population-level effects (although the heterogeneity in the effects suggests that different mechanisms are associated with different cancer sites and different patient subgroups).57DE7179, 352344Increased risk of musculoskeletal disabilityRaised body weight puts strain on the body's joints, especially the knees, increasing the risk of osteoarthritis (degeneration of cartilage and underlying bone within a joint). There is also an increased risk of low back pain.57DE7179, 352349Increased risk of heart diseaseRaised BMI increases the risk of hypertension (high blood pressure), which is itself a risk factor for coronary heart disease and stroke and can contribute to other conditions such as renal failure. The risk of coronary heart disease (including heart attacks and heart failure) and stroke are both substantially increased. Risks of deep vein thrombosis and pulmonary embolism are also increased.57DE7179, 352351Increased risk of Type 2 diabetes Obesity substantially raises the risk of Type 2 diabetes—with excess body fat estimated to underlie almost two-thirds of cases of diabetes in men and three quarters of cases in women—and people at risk of diabetes can cut their chances of getting diabetes by 60% if they lose between 5% and 7% of their body weight. Worldwide, the number of people with diabetes has tripled since 1985. [2]57DE7179, 352353Increased risk of reproductive and urological problemsObesity is associated with greater risk of stress incontinence in women. Obese women are at greater risk of menstrual abnormalities, polycystic ovarian syndrome and infertility. Obese men are at higher risk of erectile dysfunction. Maternal obesity is associated with health risks for both the mother and the child and after pregnancy.57DE7179, 352354Increased risk of sleep apnoea and asthmaOverweight and obese people are at increased risk of sleep apnoea (interruptions to breathing while asleep) and other respiratory problems such as asthma.57DE7179, 352355Increased risk of non-alcoholic fatty liver diseaseThe term ‘non-alcoholic fatty liver disease’ (NAFLD) refers to a range of conditions resulting from the accumulation of fat in cells inside the liver. It is one of the commonest forms of liver disease in the UK. If left untreated, it may progress to severe forms such as non-alcoholic steatohepatitis (NASH), fibrosis and cirrhosis. It has also been linked to liver cancer. 57DE7179, 352356Increased risk of gastrointestinal diseaseObesity is associated with: increased risk of gastro-oesophageal reflux and increased risk of gall stones.57DE7179, 352357Increased risk of psychological and social problemsThere are bi-directional associations between mental health problems and obesity, with levels of obesity, gender, age and socioeconomic status being key risk factors. Overweight and obese people can suffer from stress, low self-esteem, social disadvantage, depression and reduced libido.57DE7179, 3523581 in 5 UK children aged 10-11 are obeseThe National Child Measurement Programme (NCMP) figures for 2013/14, show that 19.1% of children in Year 6 (aged 10-11) were obese and a further 14.4% were overweight. Obese children and adolescents are at an increased risk of developing various health problems—such as asthma, cardiovascular disease and type 2 diabetes (as well as low self-esteem and depression)—and are also more likely to become obese adults.648CC79C, 399974A profound impact on the health of the populationObesity is responsible for more than 9,000 premature deaths each year in England, reduces life expectancy on average by nine years, and is a major risk factor in wide range of serious health problems including Type 2 diabetes (5 x), cancer (3 x the risk of colon cancer), and heart disease (2.5 x).57DE7179, 3999751 in 5 UK children aged 10-11 are obeseThe National Child Measurement Programme (NCMP) figures for 2013/14, show that 19.1% of children in Year 6 (aged 10-11) were obese and a further 14.4% were overweight. Obese children and adolescents are at an increased risk of developing various health problems—such as asthma, cardiovascular disease and type 2 diabetes (as well as low self-esteem and depression)—and are also more likely to become obese adults.648CC79C, 399983Increased risk of several cancersThe risk of several cancers is higher in obese people, including endometrial, breast and colon cancers. BMI is associated with cancer risk, with substantial population-level effects (although the heterogeneity in the effects suggests that different mechanisms are associated with different cancer sites and different patient subgroups).57DE7179, 399985Increased risk of musculoskeletal disabilityRaised body weight puts strain on the body's joints, especially the knees, increasing the risk of osteoarthritis (degeneration of cartilage and underlying bone within a joint). There is also an increased risk of low back pain.57DE7179, 399986Increased risk of heart diseaseRaised BMI increases the risk of hypertension (high blood pressure), which is itself a risk factor for coronary heart disease and stroke and can contribute to other conditions such as renal failure. The risk of coronary heart disease (including heart attacks and heart failure) and stroke are both substantially increased. Risks of deep vein thrombosis and pulmonary embolism are also increased.57DE7179, 399987Increased risk of Type 2 diabetes Obesity substantially raises the risk of Type 2 diabetes—with excess body fat estimated to underly almost two-thirds of cases of diabetes in men and three quarters of cases in women—and people at risk of diabetes can cut their chances of getting diabetes by 60% if they lose between 5% and 7% of their body weight. Worldwide, the number of people with diabetes has tripled since 1985.57DE7179, 399988Increased risk of reproductive and urological problemsObesity is associated with greater risk of stress incontinence in women. Obese women are at greater risk of menstrual abnormalities, polycystic ovarian syndrome and infertility. Obese men are at higher risk of erectile dysfunction. Maternal obesity is associated with health risks for both the mother and the child and after pregnancy.57DE7179, 399989Increased risk of sleep apnoea and asthmaOverweight and obese people are at increased risk of sleep apnoea (interruptions to breathing while asleep) and other respiratory problems such as asthma.57DE7179, 399990Increased risk of non-alcoholic fatty liver diseaseThe term ‘non-alcoholic fatty liver disease’ (NAFLD) refers to a range of conditions resulting from the accumulation of fat in cells inside the liver. It is one of the commonest forms of liver disease in the UK. If left untreated, it may progress to severe forms such as non-alcoholic steatohepatitis (NASH), fibrosis and cirrhosis. It has also been linked to liver cancer. 57DE7179, 399991Increased risk of gastrointestinal diseaseObesity is associated with: increased risk of gastro-oesophageal reflux and increased risk of gall stones.57DE7179, 399992Increased risk of psychological and social problemsThere are bi-directional associations between mental health problems and obesity, with levels of obesity, gender, age and socioeconomic status being key risk factors. Overweight and obese people can suffer from stress, low self-esteem, social disadvantage, depression and reduced libido.57DE7179 URL:
|
Link[5] Medical Consequences of Obesity
Author: George A. Bray
Publication info: 2004 June, 4 – Journal of Clinical Endocrinology and Metabolism. 89(6): 2583-2589
Cited by: David Price 5:07 PM 5 September 2014 GMT
Citerank: (1) 399974A profound impact on the health of the populationObesity is responsible for more than 9,000 premature deaths each year in England, reduces life expectancy on average by nine years, and is a major risk factor in wide range of serious health problems including Type 2 diabetes (5 x), cancer (3 x the risk of colon cancer), and heart disease (2.5 x).57DE7179
URL: | | Excerpt / Summary Obesity is an epidemic disease that threatens to inundate health care resources by increasing the incidence of diabetes, heart disease, hypertension, and cancer. These effects of obesity result from two factors: the increased mass of adipose tissue and the increased secretion of pathogenetic products from enlarged fat cells. This concept of the pathogenesis of obesity as a disease allows an easy division of disadvantages of obesity into those produced by the mass of fat and those produced by the metabolic effects of fat cells. In the former category are the social disabilities resulting from the stigma associated with obesity, sleep apnea that results in part from increased parapharyngeal fat deposits, and osteoarthritis resulting from the wear and tear on joints from carrying an increased mass of fat. The second category includes the metabolic factors associated with distant effects of products released from enlarged fat cells. The insulin-resistant state that is so common in obesity probably reflects the effects of increased release of fatty acids from fat cells that are then stored in the liver or muscle. When the secretory capacity of the pancreas is overwhelmed by battling insulin resistance, diabetes develops. The strong association of increased fat, especially visceral fat, with diabetes makes this consequence particularly ominous for health care costs. The release of cytokines, particularly IL-6, from the fat cell may stimulate the proinflammatory state that characterizes obesity. The increased secretion of prothrombin activator inhibitor-1 from fat cells may play a role in the procoagulant state of obesity and, along with changes in endothelial function, may be responsible for the increased risk of cardiovascular disease and hypertension. For cancer, the production of estrogens by the enlarged stromal mass plays a role in the risk for breast cancer. Increased cytokine release may play a role in other forms of proliferative growth. The combined effect of these pathogenetic consequences of increased fat stores is an increased risk of shortened life expectancy. |
Link[7] Years of life lost and healthy life-years lost from diabetes and cardiovascular disease in overweight and obese people: a modelling study
Author: Steven A Grover, Mohammed Kaouache, Philip Rempel, Lawrence Joseph, Martin Dawes - David C W Lau, Ilka Lowensteyn
Publication info: 2014 December, 5
Cited by: David Price 11:07 AM 27 December 2014 GMT
Citerank: (5) 362125Premature mortalityPremature death is more likely, in general, among obese employees than non-obese employees.57DE7179, 362138Years of life lost due to obesity57DE7179, 399974A profound impact on the health of the populationObesity is responsible for more than 9,000 premature deaths each year in England, reduces life expectancy on average by nine years, and is a major risk factor in wide range of serious health problems including Type 2 diabetes (5 x), cancer (3 x the risk of colon cancer), and heart disease (2.5 x).57DE7179, 400037Premature mortalityPremature death is more likely, in general, among obese employees than non-obese employees.57DE7179, 400047Years of life lost due to obesity57DE7179
URL: | | Excerpt / Summary Excess bodyweight was positively associated with risk factors for cardiovascular disease and type 2 diabetes. The effect of excess weight on years of life lost was greatest for young individuals and decreased with increasing age. The years of life lost for obese men ranged from 0·8 years (95% CI 0·2–1·4) in those aged 60–79 years to 5·9 years (4·4–7·4) in those aged 20–39 years, and years lost for very obese men ranged from 0·9 (0–1·8) years in those aged 60–79 years to 8·4 (7·0–9·8) years in those aged 20–39 years, but losses were smaller and sometimes negligible for men who were only overweight. Similar results were noted for women (eg, 6·1 years [4·6–7·6] lost for very obese women aged 20–39 years; 0·9 years [0·1–1·7] lost for very obese women aged 60–79 years). Healthy life-years lost were two to four times higher than total years of life lost for all age groups and bodyweight categories. |
Link[9] From evidence into action: opportunities to protect and improve the nation’s health.
Author: Public Health England
Publication info: 2014 October
Cited by: David Price 0:34 AM 9 January 2015 GMT
Citerank: (4) 348688Impacts of obesityObesity presents a significant threat to the health of the UK population and a significant drain on the nation's financial resources. 24.9% of adults in England are obese—with a body mass index of over 30—62% of adults are either overweight or obese (with a BMI of over 25), and 32% of 10–11-year-olds are overweight or obese. The annual cost of obesity to the UK is estimated to be £27bn–£46bn [1], [2]; although international comparisons suggest that the true cost could be significantly higher.57DE7179, 362629PHE – ObesityTackling obesity is one of Public Health England's key priorities to protect and improve the nation’s health.58D3ABAB, 399972Impacts of obesityObesity presents a significant threat to the health of the UK population and a significant drain on the nation's financial resources. 23% of adults are obese—with a body mass index of over 30—61% of adults are either overweight or obese (with a BMI of over 25), and 33% of 10–11-year-olds are overweight or obese. The annual cost of obesity to the UK economy has been estimated to be £27bn–£46bn [1], [2]; although international comparisons suggest that the true cost could be significantly higher.57DE7179, 399974A profound impact on the health of the populationObesity is responsible for more than 9,000 premature deaths each year in England, reduces life expectancy on average by nine years, and is a major risk factor in wide range of serious health problems including Type 2 diabetes (5 x), cancer (3 x the risk of colon cancer), and heart disease (2.5 x).57DE7179
URL:
|
|
|