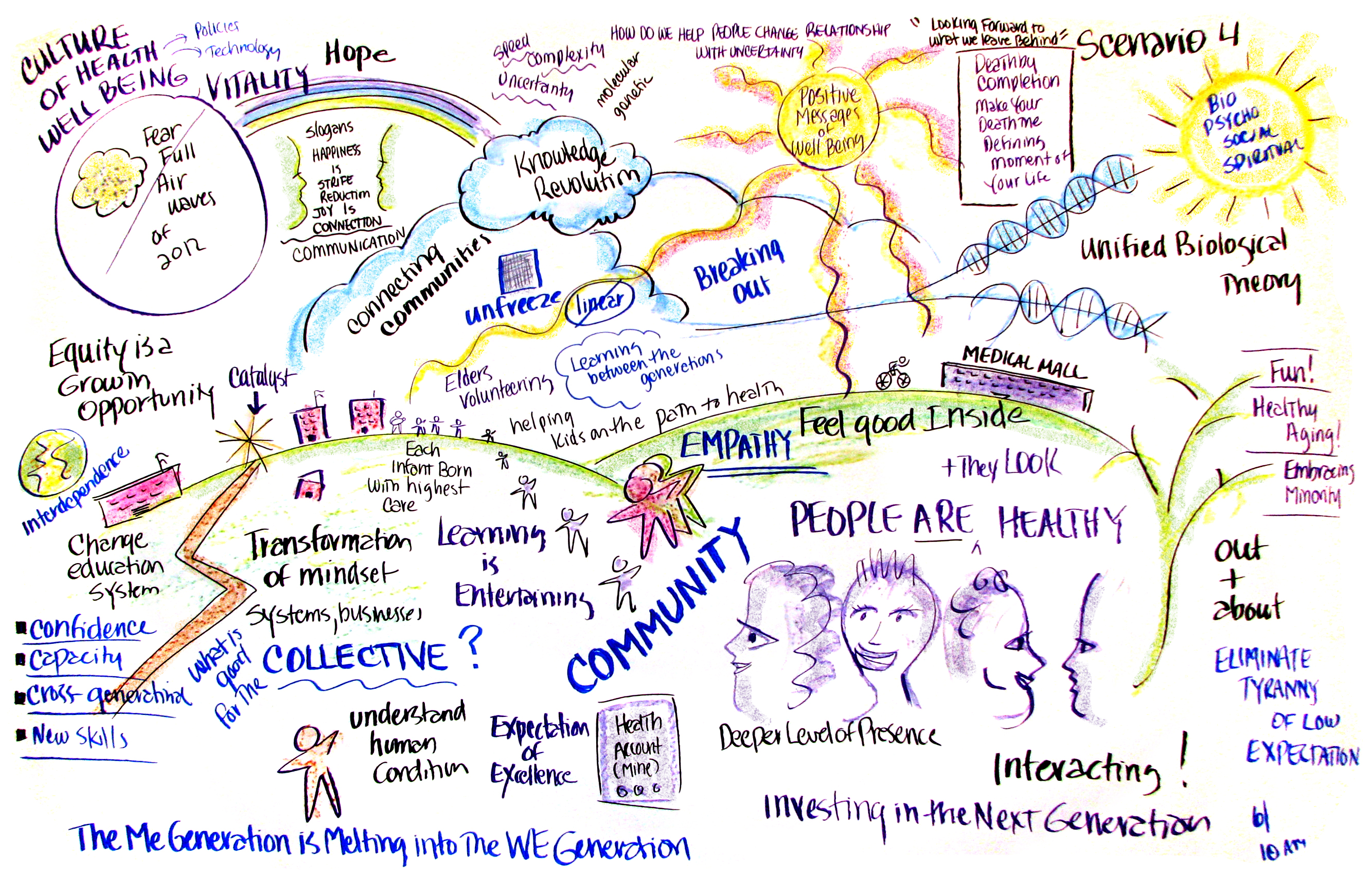
In 2032, most Americans know what only a few knew before – that the human being is a profoundly resilient organism with an innate drive for healthy growth. While familiar to the fields of psychology and spirituality, this knowledge initially encountered resistance from those focused solely on the biological mechanisms of disease. However, as systems biology evolved into a health ecology that encompassed all the domains of health, leaders across all domains of health care learned to unleash the innate human health potential by creating environments for health using a blend of federal, state, local, and private resources and methods. As people live, play, work, and pray in these environments, the benefits extend far beyond what was once considered health. In 2032, these benefits are rigorously measured and publicized, and individuals and communities that achieve the greatest health gains are lifted up as health exemplars and as cultural icons. These people and places are more innovative, creative, and economically vibrant than most and they fascinate the public.
Many attribute the emergence of these exemplars of the “health culture” in great part to the existential crisis of a huge Baby Boomer generation facing retirement and death, a crisis that began in earnest in 2012. This seemingly personal crisis played out in society, politics, and culture. For example, when a reality TV program launched in 2015 followed patients through hospice care, it captivated old and young viewers alike and prompted a public conversation about what a “good death” looks like. This conversation was furthered by news accounts of public figures refusing heroic care at the end of life and by the public reflections of celebrities dealing with terminal illness.
As they contemplated the legacy they would leave behind, many elders shifted their attention to the nation’s youth. It was becoming increasingly obvious that young people faced significant challenges in education, employment, and health, and that economic stagnation was depriving recent graduates of both the economic and psychological benefits of paid, meaningful work. Social media turned the private struggles of children and adolescents, especially around bullying, suicide, and sexuality, into topics of public discourse. Further, a steady drumbeat of stories about teens too obese to join the military, over-medicated children underperforming in school, and children living in poverty confirmed many Americans’ view that the country was failing its youth. The consequences were increasingly evident on the streets, as in a 2013 student debt protest in Los Angeles that left three college students dead.
This focus on youth helped many Americans overcome the denial that had characterized the major policy debates of the last two decades. In the Medicare debate, transparent measures of health clearly demonstrated that expenditures near the end of life came at the expense of investments made to assure children, adolescents, and young families will flourish throughout life. People connected the dots between projections for a bankrupt Medicare Trust Fund and the growing number of bankrupt families. A Medicare reform passed in 2017 that capped annual spending and used local councils to set limits on care. This led to a nationwide squeeze on any health care services that could not show a high rate of health return on dollars spent. This resulted in a sharp decline in treatments other than palliative care near the end of life, and in 2032 most elders die in their homes.
The change in demand for invasive and complex medical interventions declined not just for elders because many Americans came to see their bodies as resilient and strong. People wanted to let their bodies heal themselves whenever possible, without invasive medical or pharmaceutical interventions so healing became a popular topic in books, blogs and talk shows. Throughout the 2020s many more people came to prefer complementary and alternative medical practices that viewed the human body in this way. For many conditions, CAM practices were shown to achieve better health outcomes than traditional Western medicine, particularly when the patient experience was taken into account. This approach to the human body, which was consistent with traditional medicine in Asia, gained more momentum given the growing number of U.S. health care providers that were of Asian origin or descent.
Comparative effectiveness studies from the 2010s showed prevention and primary care also offer high health returns. Over the 2020s many communities excluded costly treatments from local offerings, meaning people had to travel elsewhere to get specialized care. A low-cost Primary Care Direct network emerged out of concierge care systems so that in most communities people find inexpensive providers for routine care. However, old routines such as annual physicals were overturned because they were less effective in promoting healthy behaviors and wasted money on tests, procedures and fees. Instead, most people use software agents such as health advocate avatars to assure optimal health. Because the world’s medical knowledge is readily available with the computational power to collect, measure, analyze and simulate personal biological and social information, health and wellness have become transparent. Most people know their status and prospects as well as those of the people around them, and people talk about the changes that matter in a way that would have been unimaginable in earlier times. When facing an illness that needs specialized care, people can go to the large medical hubs, such as Houston. However, fewer take that option than once did because it has become more culturally acceptable to avoid invasive procedures and use the softer approaches that have been popularized through different spiritual traditions. Popular culture now drives for health with an ambition that once marked the drive for wealth, and in most communities there is a strong demand that local health care providers focus less on treatment and more on health education.
While these changes in the health care system were important, community leaders recognized that health care was a relatively small part of the health equation. They also knew that they needed to leverage the positive emotions of joy, love, faith, and awe across all the domains of health in order to create the conditions in which the young are loved and the old are cherished. These leaders worked to shape the public conversation around key issues of health, wellness, and quality of life. To improve the emotional wellbeing of children, national leaders brought to scale several initiatives that had been demonstrated at the community level, including parenting classes for young parents in poor communities, arts programs for at-risk children, and the introduction of meditation into classrooms. Grandparenting Clubs formed to organize “walking schoolbuses,” mentorship programs for young parents, and early learning programs for preschoolers. The local efforts led to national supports when Congress enacted the landmark Head Start Redesign and Renewal Act of 2019, which became a cornerstone of efforts to develop a healthy young generation through the 2020s.
New curricula and teaching methods also brought integrated knowledge technologies into the learning experience that all generations now use, leveraging the remarkable findings from neuroscience showing how learning and healing occurs in the brain. The biological revolution that began in 2000 with the mapping of the human genome reached a new peak in 2029 with the articulation of the Unified Biological Systems Theory, which explained how biological systems develop and evolve toward higher levels of consciousness. The theory ties together many of the scientific advances that help identify and forecast health status for individuals, communities, and the species. Evolutionary processes once understood in relation to genes and species are now known to operate at all scales from the ecosystem of molecular life forms to the dynamics of the human cultures.
The new theories fueled significant advances in understanding the changing domain of social health. Many Americans began using social networking tools that allowed them to “crowd-source” their own health care by sharing health data with trusted friends who can alert them of issues that may warrant more attention. The website “100goodyears.org” enabled people to create and share personalized behavioral strategies to optimize their own health and longevity. Innovative public health initiatives now place “health mavens” within social networks in order to provide other members with mentorship on healthy behaviors. The widespread use of video and face-reading technologies allowed emotional wellbeing to be measured as a snapshot or over time, and has facilitated research demonstrating that the wealthy can only be healthy when they care for the poor.
In real-world communities, new methods of social and economic interaction emerged to improve social health, which has yielded benefits for community resilience and self-sufficiency. For example, time-banks offered neighbors a platform for bartering their time and services; collaborative consumption schemes allowed people access to the assets they need without having to buy their own; and peer-to-peer renting allowed people to earn income from the assets they already own. Micro-cash payments provided monetary compensation for minor contributions to a larger effort. These new platforms for interaction fostered communities in which all residents are accorded respect and meaning for the contribution they make.
These communities raised the standard for behavioral health, since residents no longer tolerated the promotion of unhealthy behaviors that create economic and health burdens for everyone. Policies in the early 2020s severely curtailed smoking, and alcohol abuse was treated with a variety of effective approaches. More significantly, new learning in behavioral health offered opportunities to promote behavior change by altering the conditions in which choice occurs. For example, so-called “food deserts” were eradicated, and agricultural subsidies for sugar and other less healthy foods were replaced with a healthy food policy that encouraged the production of foods shown to promote health. Over time, these initiatives created environments where the easy choice is the healthy choice. In addition to these changes in the environment, personalized health avatars were developed that deliver health coaching tailored to the user’s lifestyle, knowledge level, and learning style. One indicator of these changes is obesity. After two decades of steady increase ending up with from one third of Americans obese in 2010, the rate fell through the 2010s and 2020s, and by 2032 fewer than 5% of Americans are obese. Diabetes rates also declined, and for those who have diabetes it is much better controlled.
Environmental health also improved over the decades to 2032 through the reduction of major toxins and pollutants. Inexpensive environmental monitoring devices were installed throughout many communities, and built into many mobile technologies. These devices can be set to provide continuous “geotagged” health and environmental data to social networks and online mapping platforms that use new analytics to identify local factors impeding health and to point public health officials toward innovative solutions. Much of this data is automatically captured by patients’ electronic health records, which have become an interactive space for patients, health care providers, public health officials, and health avatar designers. Over time, the crowd-sourcing of environmental monitoring created greater transparency around industry practices, leading many corporations to accelerate their adoption of sustainable technologies.
Similarly, transparency improved in medical care, thanks to new payment systems originated in the early 2010s but enhanced through a series of health care reform bills that drove the integration of care and quality improvements. Further, new regulations requiring the “meaningful use” of health avatars obviated the need for a physician visit to deal with minor ailments. Both hospital payments and physician payments became tightly aligned with the value of health as an asset for creative work that sustains community economics. Biomonitoring devices provide care teams with up-to-the-minute data on a patient’s health situation allowing them to get ahead of chronic conditions and major events. When physician visits are required, they now take place in schools, workplaces, and neighborhoods, or in health homes that serve as a point of entry for a range of services that may include virtual care, telemedicine, social services, or tertiary care at regional “centers of excellence.” Payment reforms incentivized provider teams in all these settings to rapidly adopt new practices supported by comparative effectiveness research derived from a national knowledge network that supports local health improvements and helps prune unnecessary procedures that offer little value.
Improvements across all the domains of health have reduced health care spending (as traditionally defined) to 14 percent of GDP. As actuarially-based health insurance plans folded in the mid-2020s, governments created individual global lifetime health spending accounts that are sensitive to genomic variation and social determinants, and that incentivize consumers to try to “beat the odds.” People can get professional care from a variety of integrated delivery systems, including highly effective Community Health Centers, but the most important care is self-care supported by families, neighborhoods, and networked health avatars that make health knowledge available to all.